Prednisone for Eczema: Risks and Benefits
Quick Summary
- Eczema includes several types; symptoms include intense itch, redness, scaling, cracking, and discoloration that varies by skin tone.
- Prednisone is an oral steroid that can quickly reduce severe inflammation, but it doesn’t address underlying eczema drivers.
- It’s reserved for severe, widespread flares or as a short bridge while starting longer-term therapies and barrier repair.
- Courses are usually 5–14 days; improvement often starts in 24–72 hours, and tapering may be needed after longer use.
- Risks include insomnia, mood changes, high blood sugar, infection risk, and rebound flares; repeated use raises serious long-term harms.
Introduction
Understanding Eczema
Eczema is an umbrella term for inflammatory skin conditions that cause itching, redness, and a disrupted skin barrier. Many people use “eczema” to mean atopic dermatitis, but there are several types, and that matters because triggers, appearance, and treatment can differ.
Types of Eczema: Atopic dermatitis is the most common and often overlaps with allergies or asthma. Contact dermatitis is triggered by an irritant or allergy such as fragrances, nickel, or certain preservatives. Dyshidrotic eczema causes small, deep blisters on the hands and feet. Nummular eczema appears as coin-shaped patches. Seborrheic dermatitis affects oily areas like the scalp and face.
Common Symptoms: Itching is usually the main symptom and can be intense enough to disrupt sleep. Skin may look red, pink, violet, brown, or gray depending on skin tone. Flares can include scaling, rough texture, weeping, crusting, and painful cracking. Chronic scratching can thicken the skin and deepen discoloration.
In the Seattle area, cold weather, indoor heating, and frequent handwashing can worsen dryness and irritation, which can make flares feel harder to control. A good plan focuses on calming inflammation while repairing the barrier, not just suppressing itch for a few days.
Prednisone Overview
Prednisone is an oral corticosteroid, sometimes called a systemic steroid. It is a powerful anti-inflammatory medication that can calm widespread inflammation quickly, but it affects many systems in the body.
What is Prednisone? Prednisone is a prescription medication that the liver converts into prednisolone, the active form. It is used for many inflammatory conditions, including asthma flares, severe allergic reactions, autoimmune disease, and certain skin disorders.
How Prednisone Works for Eczema: Prednisone reduces immune-driven inflammation by lowering the release and activity of inflammatory signals. During a severe eczema flare, that can mean less redness, swelling, and itch within a short window. However, prednisone does not fix the underlying tendency toward eczema. If maintenance treatment and trigger control are not in place, symptoms can return quickly after stopping.
When to Consider Prednisone
Prednisone for eczema is not a first-choice option for routine flares. Dermatologists usually reserve it for select situations where rapid control is needed and there is a clear plan for what happens when the course ends.
Signs That Indicate the Need for Prednisone: A severe, widespread flare that is disrupting sleep or daily function. Significant swelling or inflammation that is not responding to appropriate topical therapy. A situation where rapid symptom control is needed while starting other longer-term therapies. Prednisone may also be used as a short bridge in carefully selected cases, for example while arranging follow-up, confirming diagnosis, or initiating steroid-sparing options.
Prednisone is most often considered when the flare is so intense that other measures are not enough on their own. Examples include widespread inflammation where applying topical medication to large body areas is not practical, severe swelling and itch that prevents sleep for several nights, or a flare that is escalating despite correct use of prescription topicals. In these cases, the goal is usually to “quiet the fire” briefly while a safer long-term plan is put in place.
A well-structured plan usually includes aggressive barrier repair at the same time: frequent fragrance-free moisturizing, gentle cleansing, and avoiding new products that can sting or trigger contact dermatitis. Many clinicians also recommend intensifying topical therapy during the course, then stepping down as the skin improves. For severe body flares, wet wrap therapy and thick moisturizers can reduce itch and help topical medications work better, which may reduce the likelihood of needing repeated oral steroid courses.
Because oral steroids can mask symptoms, follow-up matters. If flares are frequent, dermatologists often look for drivers such as contact allergy, undertreated inflammation, or bacterial overgrowth, and they may recommend steroid-sparing options like calcineurin inhibitors, phototherapy, biologic therapy, or other systemic medications rather than repeating prednisone. The goal is fewer flares and less reliance on rescue treatment. This approach is especially helpful for chronic, relapsing disease.
Equally important is when prednisone is a bad idea. If a flare is mild to moderate, topical treatment is usually safer. If there is a concern for active infection, especially viral infection, systemic steroids can worsen outcomes and should be assessed carefully by a clinician. Repeated “burst” courses can also lead to a cycle of rebound flares and escalating risk.
Comparison with Topical Treatments: Most people can manage many flares with targeted topical therapy. A topical corticosteroid treats the skin directly with far less whole-body exposure than oral steroids. Topical treatment also allows a step-up, step-down approach: higher potency for a short period on thick plaques, then a lower potency or non-steroid for maintenance.
Steroid Cream vs Hydrocortisone: Hydrocortisone is a low-potency steroid and is often used on delicate areas or for mild inflammation. Prescription steroid creams can be stronger and are selected based on location, severity, and skin thickness. The phrase “steroid cream vs hydrocortisone” can be misleading because hydrocortisone is itself a steroid. The practical difference is potency and where it is safe to use, not whether it “counts” as a steroid.
Topical Corticosteroid Options: A topical corticosteroid comes in different strengths and vehicles. A steroid ointment is often preferred for very dry, thick, or cracked eczema because ointments are more occlusive and tend to sting less than creams on inflamed skin. Creams can feel lighter and may be useful in some skin folds, while lotions and solutions can be easier for hairy areas.
A useful dosing tool is fingertip units eczema guidance. One fingertip unit is the amount of medication squeezed from a standard tube along the length of an adult fingertip, from the tip to the first crease. One fingertip unit typically covers about two adult palm-sized areas. This helps people apply enough medication to be effective, without under-treating or overusing.
Eczema Steroid Pills
Oral steroids are sometimes called eczema steroid pills. They can calm symptoms fast, but they are generally avoided as a long-term strategy for chronic eczema because the risks add up and rebound is common when stopping.
Dosage and Administration: Dosing varies based on severity, body size, other medical conditions, and clinician preference. Courses often start at a moderate dose and then taper down. Prednisone is commonly taken in the morning with food to reduce stomach upset and lower the chance of insomnia. People with diabetes, high blood pressure, glaucoma, mood disorders, or a history of ulcers may need additional monitoring and individualized decision-making.
Duration of Treatment: Dermatologists typically aim for the shortest effective course. Many courses for severe flares last about 5 to 14 days, sometimes with a taper. Longer courses increase the likelihood of side effects and raise the risk of a rebound flare when the medication ends. If someone has been on prednisone longer, tapering becomes especially important to allow the body’s natural cortisol production to recover.
How long does prednisone usually take to calm a severe eczema flare? Many people notice a reduction in itch and redness within 24 to 72 hours, with clearer improvement over the first week. The timeline depends on how inflamed the skin is, whether there is infection or a trigger still present, and whether topical care and moisturizing are supporting the skin at the same time.
Side Effects and Risks
The key issue with prednisone for eczema is not whether it can reduce inflammation. It often can. The key issue is the tradeoff, especially with repeated courses.
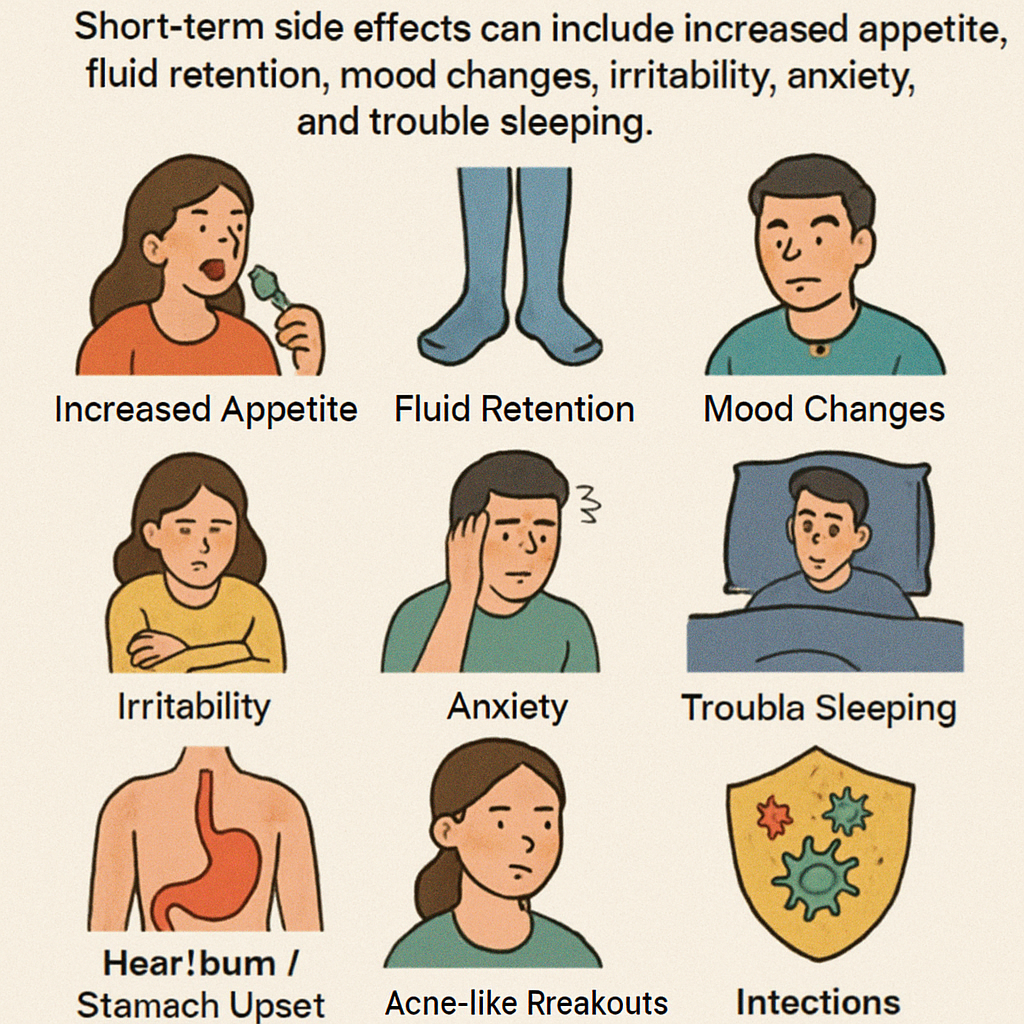
Common Side Effects of Prednisone: Short-term side effects can include increased appetite, fluid retention, mood changes, irritability, anxiety, and trouble sleeping. Some people notice heartburn or stomach upset, and acne-like breakouts can occur. Blood sugar can rise, which is especially relevant for people with diabetes or prediabetes. Because prednisone suppresses immune function, infections may be easier to catch and harder to fight while on treatment.
Serious Risks Associated with Prolonged Use: With longer or repeated use, risks become more significant. These include high blood pressure, weight gain, osteoporosis, muscle weakness, thinning skin, easy bruising, delayed wound healing, cataracts, glaucoma, and increased infection risk. Another major concern is adrenal suppression, where the body reduces its own cortisol production. Stopping steroids abruptly after longer use can be dangerous, which is why tapering plans matter.
For eczema specifically, rebound is a practical risk. The skin may calm quickly on prednisone, then flare again when the course ends if maintenance therapy is not in place. Repeated cycles can make eczema harder to manage and expose the body to more systemic steroid harm over time. This is one reason dermatologists avoid using prednisone long term for chronic eczema and instead focus on steroid-sparing strategies when flares are frequent or severe.
Conclusion
Prednisone can be appropriate for select, severe eczema flares when rapid control is necessary, but it is best viewed as a short-term bridge, not a routine fix. For many people, a carefully chosen topical corticosteroid plan, consistent moisturizer use, and trigger avoidance can manage most flares with fewer risks. Using topical steroids correctly, including appropriate strength, vehicle choice, and fingertip units eczema dosing, often makes treatment more effective and safer.
If you are needing repeated oral steroid bursts, that is a signal to reassess the overall approach. A dermatologist may consider optimizing topicals, adding non-steroid anti-inflammatory creams, evaluating for infection or contact allergy, or discussing phototherapy and systemic options that are designed for longer-term control.
Additional Resources
For reliable education and patient support, consider resources and care plans from established eczema and dermatology organizations and discuss a written flare plan with your clinician. Helpful topics to look for include:
- How to use topical steroids safely, including when to choose a steroid ointment versus a cream
- Moisturizing strategies and barrier repair basics
- Recognizing signs of skin infection during a flare
- Options beyond oral steroids for persistent disease, including newer targeted therapies
Disclaimer: This article is for general educational purposes only and does not provide medical advice, diagnosis, or treatment. Do not start, stop, or change prescription medications, including prednisone, without guidance from a qualified healthcare professional. Seek prompt medical care if you have severe symptoms, signs of infection such as rapidly worsening pain, pus, fever, spreading redness, or concerns about medication side effects.





