Unlike other types of cancer, such as melanoma or squamous cell carcinoma, basal cell carcinoma typically exhibits a slow-growing nature and seldom metastasizes, meaning it rarely spreads to distant parts of the body.
Instead, BCC tends to proliferate locally, invading nearby tissues if left untreated. While metastasis is exceptionally rare in BCC cases, it’s crucial to understand the potential for aggressive behavior and the risk factors associated with advanced disease.
Risk Factors for Metastasis
Several factors may increase the risk of aggressive or advanced basal cell carcinoma:
- Neglected or Advanced Tumors: Delayed diagnosis and treatment can allow basal cell carcinomas to progress, leading to larger and more invasive tumors with an increased risk of local spread.
- Tumor Location: Basal cell carcinomas situated on certain areas of the body, particularly those exposed to significant sun exposure, such as the head, neck, and hands, may have a higher propensity for local invasion and require more extensive treatment interventions.
- Immunosuppression: Individuals with compromised immune systems, whether due to underlying medical conditions or immunosuppressive medications, are at an elevated risk of developing aggressive or recurrent basal cell carcinomas.
- Histological Subtype: Certain subtypes of basal cell carcinoma, such as infiltrative or morpheaform BCC, are associated with a greater potential for local invasion and recurrence, although metastasis remains exceedingly rare in these cases.
Exploring Risk Factors for Metastatic Basal Cell Carcinoma
Understanding the risk factors associated with metastasis in Basal Cell Carcinoma (BCC) is crucial for early detection, accurate diagnosis, and effective treatment. While BCC typically exhibits a slow-growing and non-aggressive nature, certain factors may increase the likelihood of metastatic spread.
Here, we delve into the key risk factors implicated in the metastasis of BCC:
- Tumor Size: Larger BCC lesions are more likely to exhibit aggressive behavior and metastasize than smaller lesions. Tumors exceeding a certain size threshold, often defined as greater than 2 centimeters in diameter, are associated with an increased risk of metastasis.
- Location: The anatomical site of the BCC lesion can influence its metastatic potential. Tumors located in areas with rich vascularity or lymphatic drainage, such as the head and neck region, may have a higher propensity for metastasis due to easier access to blood and lymphatic vessels.
- Histological Subtype: Different histological subtypes of BCC exhibit varying degrees of aggressiveness and metastatic potential. While most BCCs are of the nodular or superficial subtype, aggressive variants such as infiltrative, micronodular, or morpheaform BCCs are more likely to metastasize.
- Immunosuppression: Patients with compromised immune function, either due to underlying medical conditions or immunosuppressive therapies, are at increased risk of developing aggressive and metastatic forms of BCC. Immunosuppression impairs the body’s ability to recognize and eliminate cancer cells, allowing tumors to proliferate and spread unchecked.
- Recurrent Lesions: BCC lesions that recur following previous treatment are more likely to exhibit aggressive behavior and metastasize. Recurrence may indicate underlying tumor aggressiveness or inadequate initial treatment, necessitating close monitoring and aggressive management.
- Perineural Invasion: BCC cells’ invasion of nerves, known as perineural invasion, is associated with an increased risk of local recurrence and metastasis. Tumors exhibiting perineural invasion may spread along nerve pathways, leading to distant metastases in rare cases.
- Genetic Factors: While most BCCs are sporadic and arise from cumulative sun exposure, a small subset may have underlying genetic predispositions that increase the risk of metastasis. Genetic syndromes such as basal cell nevus syndrome (Gorlin syndrome) are associated with multiple BCCs and an elevated risk of metastatic disease.
By identifying these risk factors and incorporating them into clinical decision-making, healthcare providers can better assess the likelihood of metastasis in patients with BCC. Early detection, vigilant monitoring, and tailored treatment strategies are essential for optimizing outcomes and minimizing the risk of metastatic spread in high-risk individuals.
Navigating Diagnosis and Treatment Options for Basal Cell Carcinomas
Diagnosing and treating Basal Cell Skin Cancer involves a comprehensive approach to achieving optimal outcomes while minimizing the risk of recurrence and metastasis. Here’s an overview of the diagnostic modalities and treatment options available for BCC:
Diagnosis:
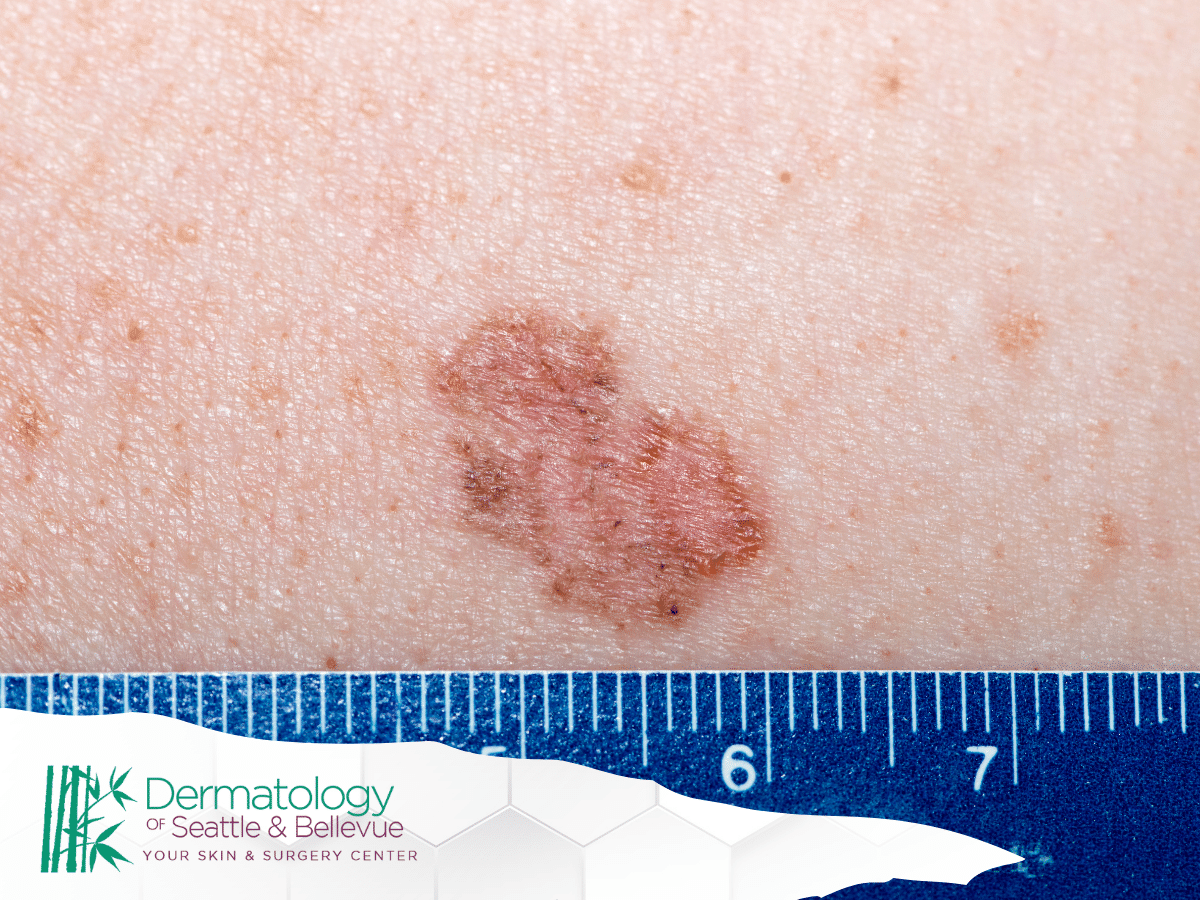
Clinical Examination: Diagnosis of BCC often begins with a thorough clinical examination by a dermatologist or healthcare provider. BCC lesions typically present as pearly or translucent nodules with rolled borders and may exhibit ulceration or crusting.
Dermoscopy: Dermoscopy, or dermatoscopy, is a non-invasive technique that allows for magnified visualization of skin lesions. Dermoscopic features characteristic of BCC include arborizing vessels, spoke-wheel structures, and ulceration.
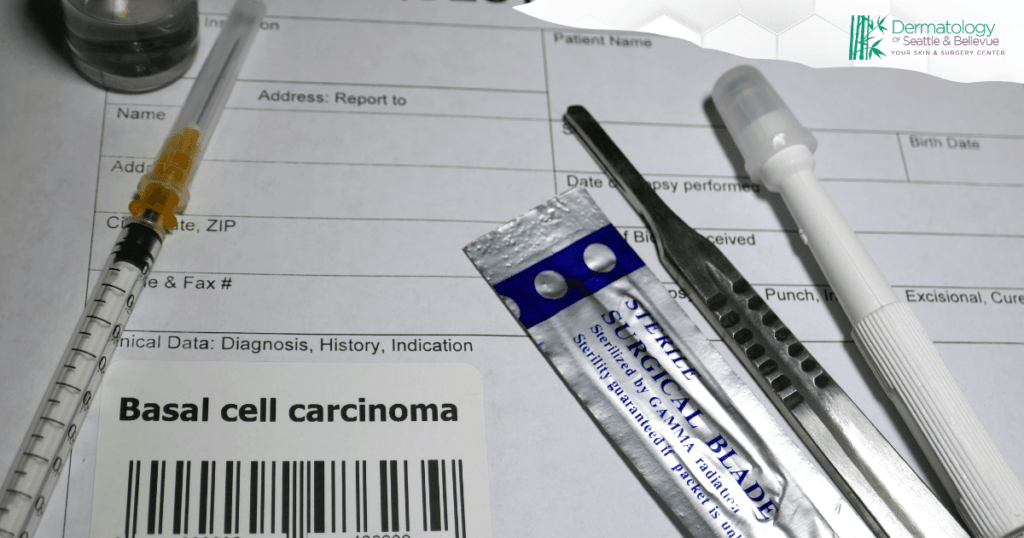
Biopsy: A skin biopsy is often performed to confirm the diagnosis of BCC and assess tumor characteristics. Depending on the size and location of the lesion, biopsy techniques may include shave biopsy, punch biopsy, or excisional biopsy.
Histopathological Examination: A pathologist examines biopsy specimens under a microscope to determine BCC’s histological subtype and assess for features such as depth of invasion, perineural invasion, and tumor margins.
Treatment:

Surgical Excision: Surgical excision remains the gold standard treatment for most cases of BCC. The tumor is surgically removed with a margin of surrounding healthy tissue to ensure complete removal and reduce the risk of recurrence. Techniques such as Mohs micrographic surgery offer high cure rates while preserving maximal healthy tissue.
Electrodesiccation and Curettage (ED&C): ED&C is a less invasive treatment option suitable for small, superficial BCC lesions. The tumor is scraped with a curette to remove the visible portion, followed by an electric current to destroy the remaining cancer cells.
Cryotherapy: Cryotherapy involves freezing the BCC lesion with liquid nitrogen to destroy cancer cells. It is typically reserved for small, superficial lesions and may require multiple treatment sessions for complete clearance.
Topical Therapies: Topical medications such as imiquimod or 5-fluorouracil (5-FU) may be prescribed for superficial BCC lesions or patients who are not candidates for surgery. These medications stimulate the body’s immune response to target and eliminate cancer cells.
Radiation Therapy: Radiation therapy, including external beam radiation therapy (EBRT) or brachytherapy, may be recommended for patients with unresectable or high-risk BCC lesions. Radiation therapy delivers targeted radiation to the tumor site, effectively destroying cancer cells while sparing surrounding healthy tissue.
Targeted Therapy: Hedgehog pathway inhibitors, such as vismodegib and sonidegib, are oral medications approved for treating locally advanced or metastatic BCC. These targeted therapies block aberrant signaling pathways involved in BCC development and progression.
Photodynamic Therapy (PDT): PDT involves applying a photosensitizing agent followed by exposure to light of a specific wavelength. This treatment selectively destroys cancer cells while minimizing damage to surrounding tissue and is often used for superficial BCC lesions.
By tailoring treatment approaches to individual patient characteristics and tumor characteristics, healthcare providers can effectively manage BCC while minimizing the risk of recurrence and metastasis. Regular follow-up and surveillance are essential for monitoring treatment response, detecting recurrence, and ensuring long-term outcomes.
Conclusion
This blog post serves as an informational resource to shed light on the metastatic potential of Basal Cell Carcinoma (BCC), its risk factors, and available diagnosis and treatment options. However, it’s essential to note that the content provided here is for educational purposes only and should not replace professional medical advice.
For the safest and most accurate information tailored to individual cases, scheduling an appointment with a qualified healthcare provider is recommended. Early detection, proper diagnosis, and personalized treatment plans are key to effectively managing BCC and ensuring optimal outcomes.