Lip skin is thin, exposed, and constantly moving, so irritation can escalate fast. If you are dealing with stinging, flaking, or persistent dryness at the mouth line, the right approach can help. This guide explains what lip eczema is, why flare-ups happen, and how to choose products that support healing without adding triggers. You will learn which ingredients tend to help, which ones often backfire, and how to build a simple routine you can stick to. If you are searching for a lip eczema ointment that feels soothing and protective, the sections below will help you narrow the options and use them correctly.
- Lip eczema often involves a damaged skin barrier, so protecting and sealing in moisture matters.
- Fragrance, flavorings, and “tingly” lip ingredients can worsen irritation.
- Ointments often work better than lotions for cracked, inflamed lips because they reduce water loss.
- Patch-testing and keeping a short ingredient list can help identify triggers.
- At-home habits, like avoiding lip licking and using gentle cleansers, support long-term control.
Understanding Lip Eczema
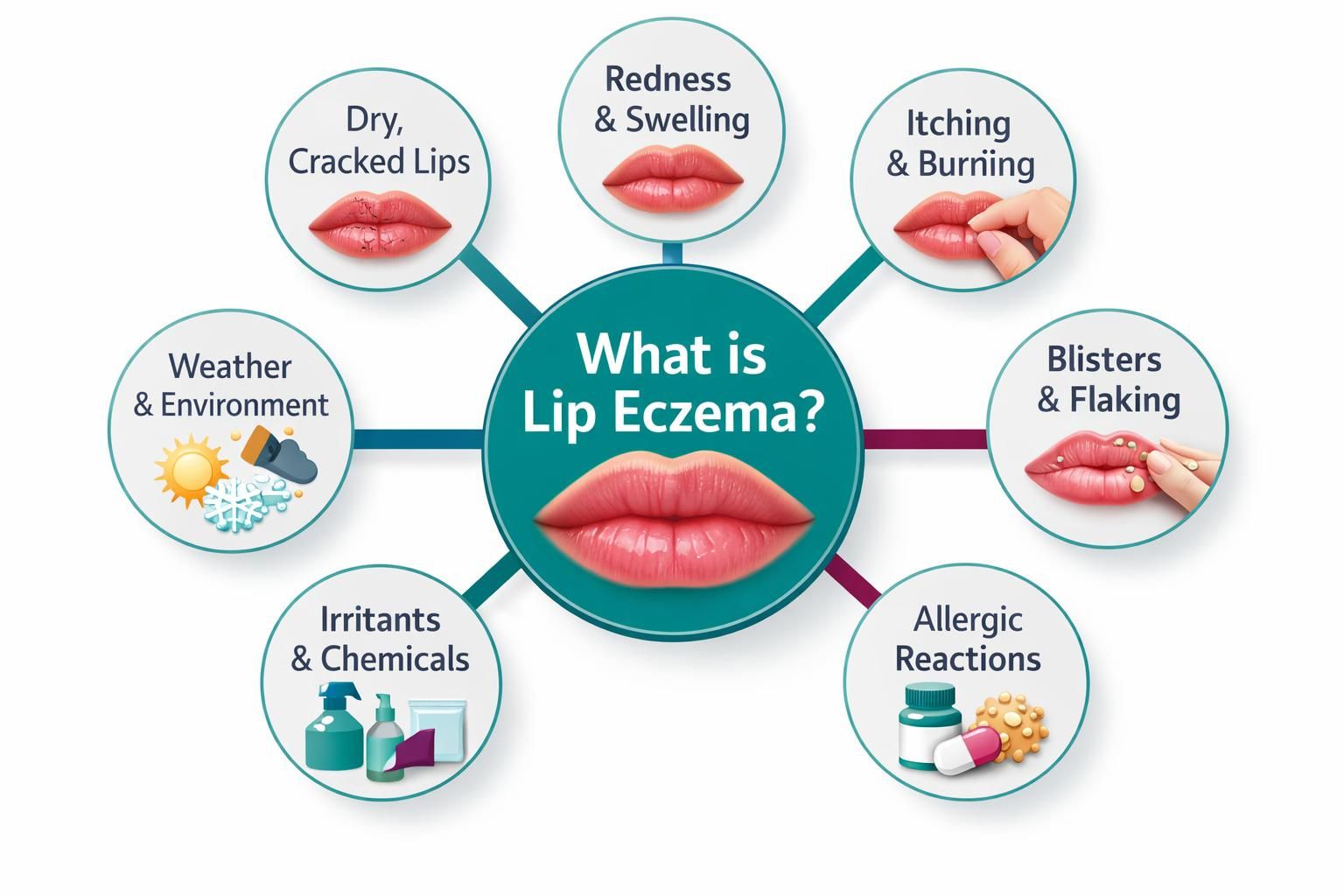
Lip eczema is irritation and inflammation affecting the lips, mouth corners, and skin around the lip line. It often flares with weather changes, saliva exposure, and harsh products. Because lips have fewer oil glands, they lose moisture quickly, so once the barrier is stressed, dryness and cracking can worsen quickly.
Many cases involve atopic dermatitis, contact dermatitis, or both. Triggers can be internal (eczema-prone skin) and external (ingredients in lip products). Knowing which pattern fits helps you choose products that calm a flare instead of feeding it.
What is lip eczema?
Lip eczema is inflammation on the lips and nearby skin that can cause redness, scaling, cracking, and discomfort. With atopic dermatitis, the barrier is naturally drier and more reactive. With contact dermatitis, a specific irritant or allergen causes a reaction after exposure.
Common triggers include fragrance, essential oils, flavorings, certain preservatives, and sometimes lanolin. Even “natural” balms can irritate if they rely on plant extracts you do not tolerate. The goal is to reduce inflammation and rebuild the barrier, not to create a cooling, plumping, or minty sensation.
Can you get eczema on your lips?
Yes. Eczema can show up mainly on the lips or as part of broader eczema. Some people flare around the mouth due to saliva, toothpaste, cosmetics, or sunscreen. Others notice it with seasonal shifts when the barrier becomes fragile.
If flares track with a specific product (lip balm, toothpaste, sunscreen, lipstick), contact dermatitis is more likely. If you also have eczema elsewhere, an atopic pattern may be involved. In both cases, a gentle routine and simple formulas are a strong starting point.
Common symptoms of eczema on lips
Lip eczema can feel worse than it looks. Symptoms may start as tightness, mild burning, and sensitivity, then progress to peeling and cracking. Strong flares can involve swelling and painful splits, especially at the corners.
Common symptoms include:
- Dryness, scaling, or flaking
- Itching, burning, or a raw feeling
- Redness or discoloration around the lip line
- Cracks, fissures, or splits
- Worsening after lip licking, spicy foods, or fragranced products
If you see crusting, spreading redness, increasing pain, or signs of infection, seek clinician guidance.
Treatment Options
A good plan combines trigger avoidance, barrier repair, and short-term anti-inflammatory support when needed. Many people cycle through balms that feel soothing at first but worsen irritation over time, often due to fragrance, flavor, menthol, or botanicals.
For many, the simplest approach works: remove likely irritants, use one bland protective product consistently, and give the barrier time to recover. If symptoms persist or keep returning, professional evaluation can help rule out allergy, infection, angular cheilitis, or other lip conditions.
Overview of eczema on lips treatment
Treatment usually starts with identifying and removing triggers. Common culprits include mint or whitening toothpaste, fragranced or flavored lip products, some sunscreens, and long-wear lip color. After trigger reduction, focus on moisturizing and sealing to limit water loss, which is where ointments help most.
During inflamed flares, a clinician may recommend short-term anti-inflammatory options. Keep ingredients minimal, avoid “active” sensations, and avoid changing products frequently. Consistency makes it easier to see what is helping.
The role of lip eczema ointment
A lip eczema ointment is often the best choice during cracking because it forms a protective layer that reduces water loss. Compared with creams, ointments usually contain less water and fewer preservatives, so they often sting less on raw skin. They also shield lips from saliva, wind, and friction.
Some people react to waxes, lanolin, or certain plant oils. A practical strategy is to start with a bland, fragrance-free option. If your lips calm down and stay calmer, keep it as your baseline.
Top Recommended Lip Eczema Ointments

The best product is usually the one you can tolerate and use consistently. For many people, that means fragrance-free, flavor-free formulas with short ingredient lists. Thicker ointments tend to work best during fissures, while a gentle lip eczema cream may feel easier in daytime once the flare improves.
Think in roles. One product seals and protects. If your lips tolerate it, a lighter moisturizer can go underneath, then be sealed with an ointment on top.
Ingredients to look for
Look for low-irritant ingredients that support the barrier and reduce water loss:
- Petrolatum: strong occlusive protection and usually well-tolerated
- Mineral oil: gentle occlusion and slip for cracked areas
- Dimethicone: barrier support and smoother feel
- Ceramides: barrier support in creams and balms
- Glycerin: humectant hydration, best when sealed with an occlusive
- Colloidal oatmeal: soothing support for itchy, reactive skin in some formulas
Ingredients that often cause trouble include fragrance, flavorings (mint, citrus), essential oils, menthol, camphor, and “plumping” agents. For most people, control comes from simplicity, not stronger sensations.
Product reviews
Choosing by formula type can be more reliable than chasing a specific brand, since reactions vary.
Plain petrolatum-based ointments: Often first-choice for acute cracking because they seal well and typically sting less than watery products. Apply a thin layer and reapply after eating, drinking, or brushing teeth.
Ceramide-based sensitive-skin balms or creams: Useful once the flare calms down, especially for daytime. Stick to fragrance-free options with simple ingredient lists.
Oat-based soothing ointments: Can help itch for some people. Patch-test if you are sensitive.
Lanolin-based products: Very protective for some, but others develop irritation. Avoid during active inflammation if you suspect sensitivity, or test cautiously.
How to Treat Eczema on Lips at Home
Home care focuses on reducing irritation and keeping conditions stable so the skin can heal. What touches your lips, how often you reapply protection, and whether you lick your lips can affect whether a flare resolves or lingers. During healing, use fewer products and repeat the basics.
Treat the surrounding area gently, too. Harsh cleansers, exfoliants, acne treatments, and fragranced skincare can migrate to the lip line and trigger symptoms. Keep your routine bland for a couple of weeks to spot triggers and support the barrier.
Natural remedies
Natural remedies can be tempting, but “natural” does not always mean gentle. If you want a simple approach, prioritize low-risk, fragrance-free options and skip essential oils and plant-heavy blends. A bland occlusive can still be the backbone of care, even if you prefer a minimal routine.