Spotting and treating rosacea flare-ups when the temperature dips is a year-round concern for many patients in cooler climates. Rosacea is a chronic inflammatory skin disorder that causes redness, visible blood vessels, and sometimes acne-like pimples on the face. Cold weather, dry air, and sudden shifts between indoor heating and outdoor chill are common triggers for flare, making winter one of the most challenging times to manage rosacea symptoms.
Quick Summary
- Cold weather, dry air, and rapid temperature changes can trigger rosacea flare-ups, causing facial redness, visible blood vessels, and acne-like bumps, often worsening in winter.
- Early flare signs include warmth, tingling, subtle flushing, and small red bumps; ocular rosacea may cause eye dryness, burning, watery eyes, or swollen eyelids and needs prompt evaluation.
- Common triggers include cold wind, stress, spicy foods, hot drinks, alcohol, sun exposure, and harsh skincare products; tracking triggers helps reduce flare frequency.
- Management focuses on gentle, fragrance-free skincare, barrier-supporting moisturizers, daily mineral sunscreen, and lifestyle adjustments like stress reduction and avoiding known dietary triggers.
- Dermatologist-guided treatments may include topical or oral medications and laser/light therapies for persistent redness and visible vessels, and diagnosis is important because rosacea can mimic acne, psoriasis, or dermatitis.
Understanding Rosacea as an Inflammatory Skin Disorder
Rosacea is more than occasional redness—it’s a long-term inflammatory skin disorder that often affects the cheeks, forehead, nose, and chin. Patients may experience flushing, visible blood vessels, or even thickened skin in more advanced cases. The condition is unpredictable, with flare cycles influenced by environmental triggers, stress, and skin sensitivity. While there’s no cure for rosacea, dermatology experts emphasize that effective treatment and prevention strategies can significantly reduce flare frequency and improve skin health.
Common Rosacea Symptoms and How They Appear on the Face
Rosacea symptoms vary, but most patients notice recurring patterns, such as:
- Facial redness: Often on the central face, especially cheeks and nose.
- Visible blood vessels: Fine red lines that become more noticeable during a flare.
- Pimples and acne-like bumps: Sometimes mistaken for traditional acne, but without blackheads.
- Oily skin or sensitive skin: Common alongside redness and inflammation.
- Eye irritation: In cases of ocular rosacea, patients may notice dryness or burning sensations.
Recognizing these rosacea symptoms early helps patients track common triggers and seek timely dermatology consultation before the condition worsens.
Spotting the Early Signs of a Rosacea Flare
Catching a rosacea flare early allows patients to minimize discomfort and reduce visible redness. Warning signs often include increased warmth or tingling in the face, subtle flushing after meals or drinks, and small red bumps appearing on sensitive skin areas. For some, ocular rosacea may present with irritated eyes or burning before skin symptoms emerge. Tracking these early signals helps patients adjust skincare routines or avoid triggers before the flare worsens.
Common Triggers: Weather, Stress, and Spicy Foods
Although every patient responds differently, certain common triggers are linked to rosacea flare patterns:
- Weather: Cold wind, winter chill, or sudden changes in temperature.
- Stress: Emotional or physical stress can quickly provoke flare activity.
- Dietary triggers: Hot beverages, alcohol, and spicy foods frequently worsen redness.
- Sun exposure: Even mild sun exposure may intensify facial redness.
- Skin care products: Harsh cleansers or cosmetics may irritate sensitive skin.
By identifying and limiting exposure to these triggers, patients can better manage rosacea symptoms throughout the year.
Ocular Rosacea: Eye Irritation and Other Signs to Watch
Ocular rosacea occurs when rosacea affects the eyes, leading to redness, dryness, and irritation. Symptoms can include watery eyes, burning sensations, swollen eyelids, or sensitivity to light. Left untreated, ocular rosacea may cause vision issues in severe cases. Dermatology and eye care specialists recommend patients experiencing eye irritation alongside facial redness book an appointment promptly for proper diagnosis and treatment options.
Erythematotelangiectatic Rosacea and Persistent Redness
One of the most common forms of rosacea is erythematotelangiectatic rosacea, marked by persistent redness and visible blood vessels across the cheeks, nose, and forehead. Unlike temporary flushing, this redness doesn’t fade quickly and can become permanent without proper treatment. Patients with this subtype often experience facial redness that worsens during flare episodes, particularly in cold weather. A dermatologist can recommend rosacea treatments such as topical medications or laser therapy to reduce the appearance of persistent redness and improve skin health.
Diagnosis and Questions to Ask Your Dermatologist
Accurate diagnosis is key, as rosacea can mimic other conditions like acne, psoriasis, or atopic dermatitis. During an appointment, patients should ask:
- What subtype of rosacea do I have?
- What rosacea symptoms should I watch for to spot a flare?
- Which triggers are most relevant for my sensitive skin?
- What treatment options work best for my specific condition?
- Are there any long-term prevention strategies I should follow?
Bringing these questions to a consultation ensures that patients leave with clear, trustworthy health information and a personalized treatment plan.
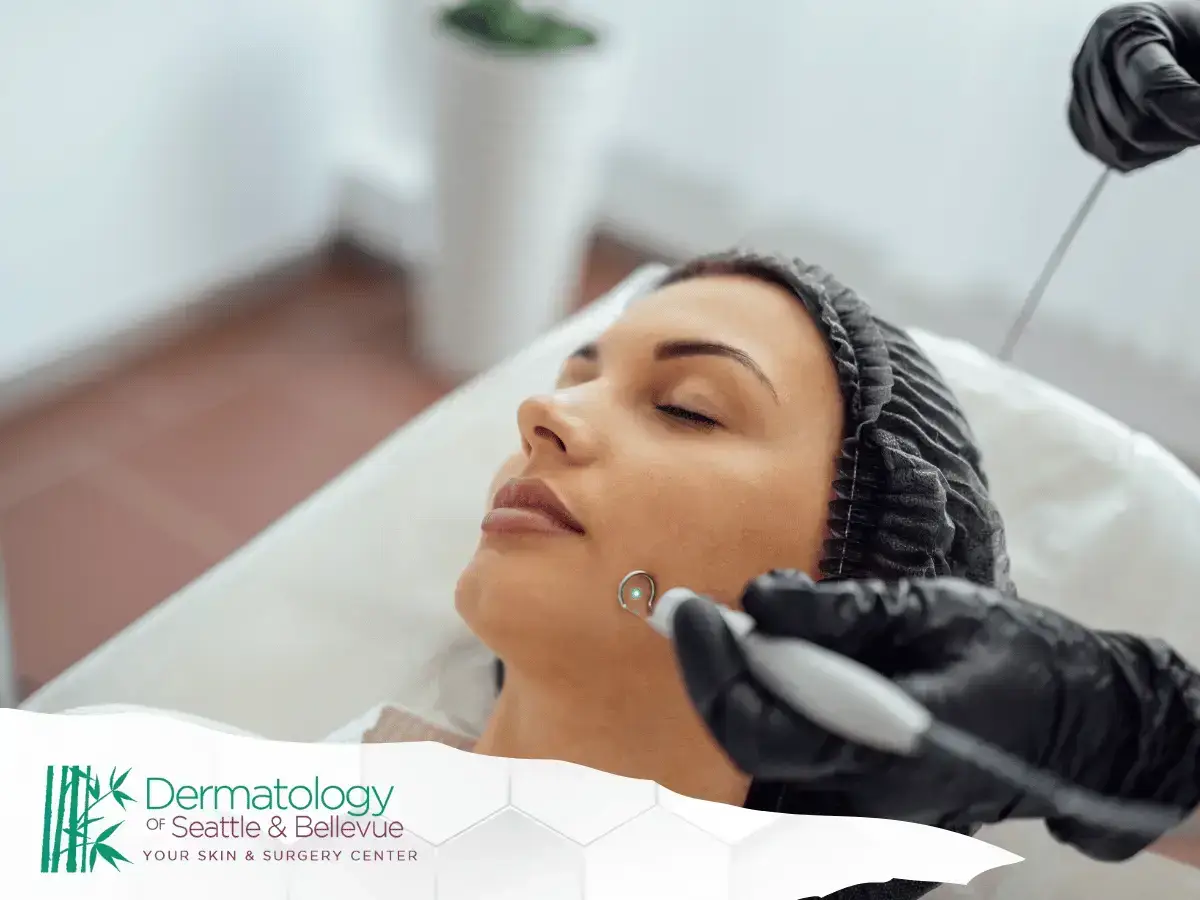
Treatment Options: Topical Medications, Sunscreen, and Gentle Skincare
Rosacea treatments vary depending on severity, but common options include:
- Topical medications: Reduce inflammation and minimize redness during a flare.
- Sunscreen: Broad-spectrum sunscreen prevents flare-ups triggered by sun exposure and lowers long-term risks like skin cancer.
- Gentle skincare: Switching to fragrance-free, soothing products helps reduce irritation.
- Lifestyle adjustments: Avoiding spicy foods, alcohol, and extreme weather changes may limit rosacea symptoms.
For patients with severe rosacea, additional treatment options like laser therapy or prescription oral medications may be considered.
Rosacea Treatments vs. Other Skin Conditions Like Acne and Psoriasis
Because rosacea shares symptoms with acne, psoriasis, and atopic dermatitis, patients often mistake it for another inflammatory skin disorder. Unlike acne, rosacea does not cause blackheads, and unlike psoriasis, it is not marked by thick, scaly plaques. A dermatologist can perform a diagnosis to confirm whether redness, pimples, or visible blood vessels are linked to rosacea. This distinction is critical since treatment strategies differ and mismanaging flare episodes can worsen the condition.
Tips for Prevention and Daily Skin Care Routine
Preventing a rosacea flare in winter requires consistency. Patients with sensitive skin should keep a gentle skincare routine that emphasizes hydration and barrier protection. Helpful tips include:
- Using a free moisturizer formulated for sensitive skin to lock in hydration.
- Applying sunscreen daily, even on cloudy days, to protect against sun exposure.
- Choosing cosmetics designed for sensitive skin to avoid unnecessary irritation.
- Washing the face with lukewarm water to avoid triggering redness.
By following these prevention strategies, patients can reduce rosacea symptoms and enjoy clearer skin through the colder months.
Stress Management and Lifestyle Adjustments for Flare Control
Stress is a well-documented trigger for flare episodes, making stress management a valuable part of any treatment plan. Practices like yoga, meditation, or even regular walks can help keep flare intensity under control. Avoiding spicy foods and alcohol, both common triggers, also supports long-term skin health. For patients dealing with ocular rosacea, lifestyle changes combined with medical treatment may reduce eye irritation and improve comfort.
Managing Rosacea in Winter and Cold Weather
Cold, dry air and wind can trigger a rosacea flare by stressing the skin barrier. When temperatures dip, protect exposed areas of skin with a soft scarf, avoid very hot showers, and switch to lukewarm water for cleansing. Indoors, reduce rapid temperature swings (for example, moving from blasting heat to outdoor chill) and run a humidifier to maintain moderate humidity. Consistent, gentle skin care helps stabilize redness and reduce the intensity of seasonal flare episodes.
Sun Protection and Skin Health Considerations
Even in winter, UV exposure can aggravate rosacea. Practice sun protection daily: apply a mineral-based SPF to the face, reapply when outdoors for extended periods, and wear wide-brim hats or UPF accessories. Mineral filters (zinc oxide/titanium dioxide) tend to be better tolerated by sensitive skin. Combine shade-seeking habits with barrier-supporting moisturizers to keep facial redness in check during bright, reflective winter days.
Cosmetics and Free Moisturizer Choices for Sensitive Skin
- Choose fragrance-free moisturizer labeled for sensitive skin to support the barrier and minimize irritation.
- Prefer simple formulas with ceramides, glycerin, and niacinamide; avoid drying alcohols and strong acids on flare-prone areas of skin.
- Select non-comedogenic, green-tinted correctors to visually neutralize facial redness without heavy coverage.
- Patch-test new cosmetics on a small area of face or jawline for 24 hours before full application.
- Remove makeup with a gentle, non-foaming cleanser; avoid harsh scrubs that can worsen a rosacea flare.
Severe Rosacea, Visible Blood Vessels, and Treatment Options
When persistent redness, flushing, and visible blood vessels interfere with daily life, discuss advanced treatment options with a dermatologist. Prescription topical medications can calm inflammatory bumps; oral therapies may be appropriate for more extensive disease. Device-based care (e.g., vascular lasers or light-based therapy) can target dilated vessels and reduce background redness over a series of sessions. For coexisting ocular rosacea, coordinate care with an eye specialist to protect vision and comfort.
Questions Patients Commonly Ask About Rosacea Symptoms
Many patients wonder whether burning, stinging, and intermittent pimples are part of rosacea—yes, these symptoms can occur during a flare. Others ask how quickly a trigger (like hot beverages or spicy foods) can set off flushing—often within minutes. People also ask whether there’s a cure for rosacea—there isn’t a permanent cure, but consistent management and tailored treatment can control signs and reduce flare frequency. Finally, patients frequently ask how long to expect improvement—most see steadier skin within weeks of adopting gentle routines and prescribed care.
Privacy Terms, Manage Settings, and Trustworthy Health Information
- Use clinic portals that clearly outline privacy terms and how your data is stored and shared.
- Review “manage settings” options for messaging, photo uploads, and telederm visits so you control what’s visible to care teams.
- Rely on trustworthy health information from board-certified dermatology sources and established medical organizations; avoid unvetted advice that promises instant fixes.
- When booking an appointment online, verify secure checkout and confirmation details, and save copies of forms for your records.
Conclusion: Finding Relief and Control Over Rosacea Flare-Ups
Effective control starts with identifying triggers, recognizing early rosacea symptoms, and committing to gentle routines that protect the skin barrier. Layer daily sun protection, calming moisturizers, and stress management with dermatologist-guided care to reduce flare intensity and duration. By personalizing habits to your environment and skin, you can navigate colder months with fewer setbacks and greater comfort.
Disclaimer: Educational Purposes Only
This content is for informational purposes only and does not replace professional medical advice. Always consult a licensed dermatologist or qualified healthcare provider for diagnosis, individualized treatment, and guidance tailored to your medical history and skin.