Skin cancer is a broad term for cancers that begin in the skin, often after years of sun exposure, though other factors also contribute. Understanding melanoma vs carcinoma helps explain why some lesions need faster treatment and why doctors use different terms. In general, carcinoma refers to cancers starting in the upper skin layers, while melanoma starts in pigment-producing cells and can behave more aggressively. This guide covers the most common types, how they tend to look and grow, and what diagnosis and treatment typically involve.
- Carcinoma commonly includes basal cell and squamous cell cancers, which often grow locally first.
- Melanoma arises from melanocytes and is more likely to spread if not caught early.
- Appearance can overlap, so change over time matters as much as a single snapshot.
- A skin exam plus biopsy is the usual pathway to a definitive diagnosis.
- Treatment ranges from minor procedures to wider surgery and additional therapies depending on type and stage.
Introduction to Skin Cancer
Skin cancer develops when skin cells grow in an uncontrolled way. It often begins in frequently sun-exposed areas such as the face, scalp, ears, neck, forearms, and hands, but it can also appear on less-exposed skin. Genetics, immune status, tanning beds, and a history of sunburns can influence risk.
In skin cancer, “carcinoma” usually refers to basal cell carcinoma (BCC) and squamous cell carcinoma (SCC), often grouped as non-melanoma skin cancers. Melanoma is different because it starts in melanocytes (pigment cells) and can spread differently, which affects urgency and treatment.
h2Types of Skin Cancer Most discussions center on three major types: BCC, SCC, and melanoma. They differ by the cell type they originate from, how they commonly present, and how likely they are to invade deeper tissues or spread.
Because “carcinoma” is broad, many comparisons of melanoma vs carcinoma are really melanoma vs BCC or melanoma vs SCC. Knowing the basics helps explain common comparisons like basal cell versus squamous cell cancer or bcc vs melanoma.
Basal Cell Carcinoma (BCC)
Basal cell carcinoma arises from basal cells in the lower epidermis. It is the most commonly diagnosed skin cancer and often grows slowly. If untreated, it can still cause local damage, especially on the nose, eyelids, or ears.
BCC may look like a shiny, pearly bump; a pink patch; or a sore that heals and returns. Some resemble a small scar or a firm, waxy area. Because lesions can be subtle and painless, they may be mistaken for irritation. Bleeding, crusting, or ongoing change should be checked.
Squamous Cell Carcinoma (SCC)
Squamous cell carcinoma begins in squamous cells nearer the skin surface and often develops on sun-damaged areas such as the face, scalp, and backs of the hands. It commonly appears as a scaly, rough patch, a firm red bump, or a crusting or bleeding lesion.
SCC is more likely than BCC to grow deeper and has a higher chance of spreading, particularly on higher-risk sites or in people with weakened immune systems. Many SCCs are highly treatable when found early, so persistent rough spots or non-healing sores deserve evaluation.
Melanoma
Melanoma starts in melanocytes, the cells responsible for pigment. It can arise from an existing mole or develop on previously normal skin. While less common than BCC or SCC, melanoma is treated with greater urgency because it can spread to lymph nodes and other organs.
Melanoma may look like a new dark spot, a changing mole, or a lesion with multiple colors. Some are pink, red, or skin-colored, making them easier to miss. Watch for evolution: growth, shape change, color variation, or new symptoms such as itching or bleeding.
Key Differences Between Melanoma and Carcinoma
When people search melanoma vs carcinoma, they usually want to know why the names and treatment plans differ. The distinction begins with the cell of origin and shows up in growth behavior, spread risk, and typical appearance.
Overlap is common, and appearance alone cannot reliably distinguish melanoma from carcinoma. Pay attention to what is new, changing, or not healing, and get it evaluated. A biopsy provides the diagnosis.
Growth Patterns
BCC usually grows slowly and tends to stay near where it started, though it can invade nearby tissue if ignored. SCC often grows faster and can invade deeper layers more readily. Both can cause serious local damage if treatment is delayed.
Melanoma growth varies. The concern is that melanoma can spread beyond the skin earlier, which is why prompt evaluation matters.
Risk Levels
Risk depends on more than cancer type: location, size, duration, and immune suppression can all matter. Still, melanoma is generally considered the most dangerous common skin cancer because of its metastatic potential.
Carcinomas are not automatically safe. BCC rarely spreads but can be locally destructive, and SCC can metastasize in certain settings. Avoid self-triage based on assumptions or a single photo.
Appearance
The ABCDE approach for pigmented lesions (asymmetry, border irregularity, color variation, diameter change, evolving) can help flag possible melanoma, but it is not perfect.
Carcinomas often appear as non-healing sores, scaly patches, or pearly bumps, but can mimic eczema, scars, warts, or pimples. Signs that warrant a check include:
- A sore that does not heal within several weeks
- A lesion that bleeds, crusts, or oozes repeatedly
- A spot that is new in adulthood and continues to change
- A growth with persistent tenderness, itching, or an unusual sensation
BCC vs. Melanoma: A Closer Look

The bcc vs melanoma comparison is common because BCC is often described as common and slow-growing, while melanoma is less common but higher risk. Both require attention, but the urgency and follow-up may differ.
BCC often looks like a pearly, translucent bump with visible small blood vessels, or a pink patch that slowly expands. Melanoma more often shows pigment irregularity or a changing mole, but it can also be non-pigmented. Because of overlap, clinicians consider your history, lesion behavior, and exam findings, and confirm with biopsy when needed.
Diagnosis and Treatment Options
Diagnosis starts with a careful skin exam and your observations: when a spot appeared, how it has changed, and whether there is bleeding, pain, or itching. Clinicians also assess risk factors such as sun exposure history, family history, many moles, and prior skin cancers.
Treatment depends on the confirmed type and, for melanoma, how deep it is and whether there are signs of spread. Even within “carcinoma,” management differs, which is why basal cell versus squamous cell cancer comparisons matter. The goal is complete cancer removal or destruction while preserving function and appearance when possible.
Diagnostic Procedures
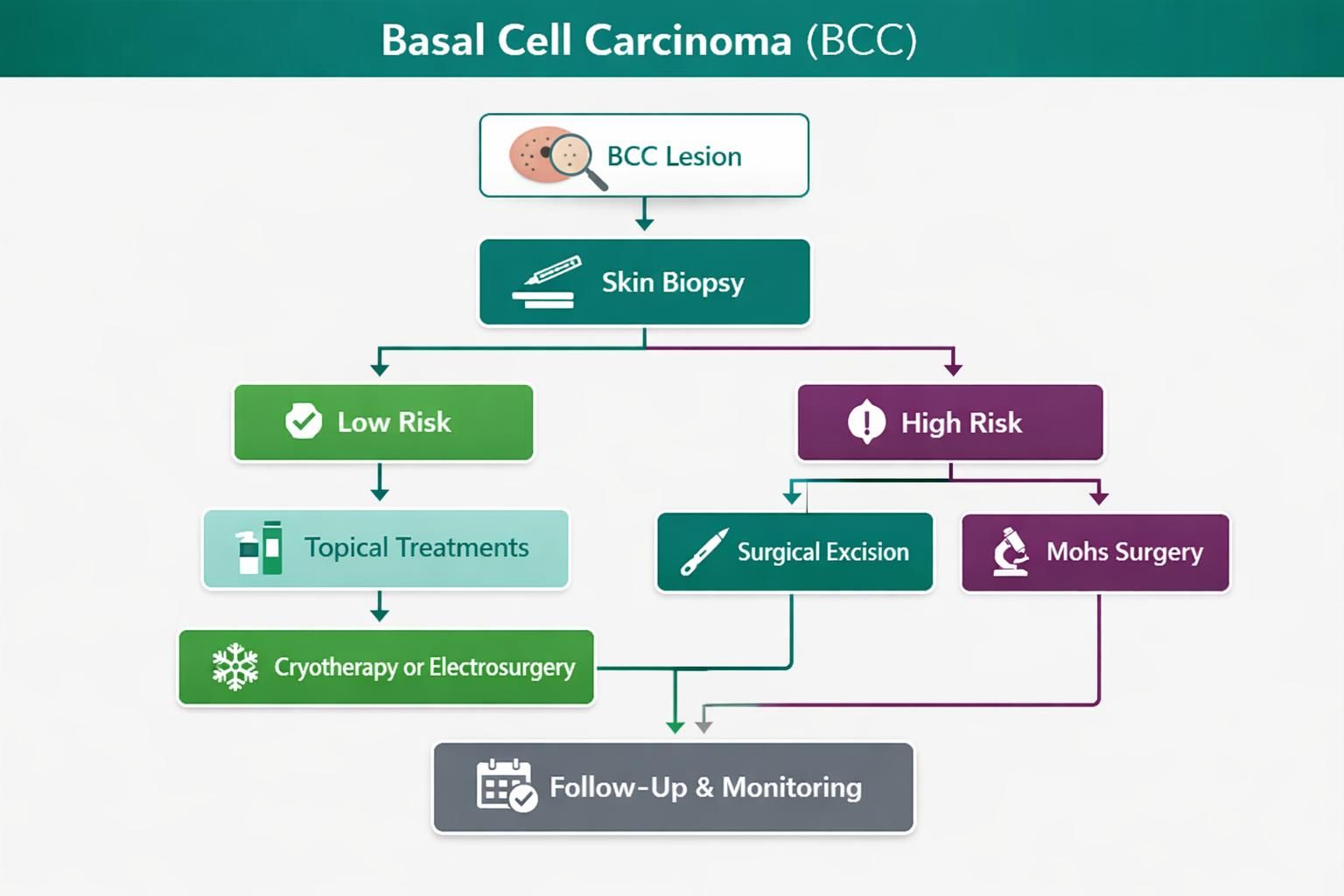
A skin biopsy is the standard way to diagnose suspected skin cancer. A clinician removes a small sample or sometimes the entire lesion, and a pathologist examines it under a microscope. The biopsy approach depends on size, location, and getting enough tissue for accuracy.
A full-body skin exam may be done to look for other suspicious areas. For melanoma, additional evaluation may be considered based on tumor features. Photos can document change over time, but they do not replace an in-person exam or biopsy when a lesion is concerning.
Treatment for BCC and SCC
Many BCC and SCC lesions are treated with procedures designed for complete removal, such as surgical excision or specialized techniques for high-risk areas like the face. Some superficial lesions may be treated with surface-directed approaches when appropriate for the tumor’s features.
Follow-up matters because having one carcinoma increases the chance of developing another. Prevention strategies





