Introduction
Eczema can be frustrating because it is not just about dry skin. The itch can dominate your day, disrupt sleep, and make it hard to focus on anything else. It is also common to hear people ask does benadryl help eczema when itching is at its worst, especially at night. In this article, you will learn what Benadryl is, how it works in the body, and whether it meaningfully improves eczema symptoms or mainly helps you feel sleepy. You will also get practical ways to reduce scratching, understand possible side effects, and explore other treatments that often address the root causes of eczema flare-ups.
- Benadryl may make you sleepier, which can indirectly reduce nighttime scratching
- Eczema itch is complex and not always driven by histamine, so antihistamines do not help everyone
- Topical Benadryl is usually not a first-choice option for eczema-prone skin
- Consistent moisturizing and anti-inflammatory topicals are often more effective for flares
- Breaking the itch-scratch cycle takes both skin care and behavior strategies
Overview of Eczema
Eczema, often used to describe atopic dermatitis, is a long-term inflammatory skin condition linked to a weakened skin barrier and an overreactive immune response. When the barrier is disrupted, skin loses moisture and becomes more vulnerable to irritants, allergens, and microbes. This can lead to dryness, redness, rough patches, and intense itching.
Symptoms can come and go in cycles, with flare-ups triggered by things like harsh soaps, sweating, scratchy fabrics, stress, temperature changes, fragrances, and some allergens. Because eczema is driven by multiple factors, the best treatment plan usually combines barrier repair, inflammation control, and trigger management rather than relying on a single medication.
Common Treatments for Eczema
Most eczema treatment plans start with daily moisturizing and gentle skin care to repair the barrier. During flares, anti-inflammatory medications are often added to calm redness and itching. Depending on severity and where eczema appears, treatments may range from over-the-counter products to prescription therapies.
Common approaches include topical corticosteroids, topical calcineurin inhibitors, prescription nonsteroidal creams, and in some cases light therapy or systemic medications. Lifestyle adjustments matter too, such as switching to fragrance-free products, using lukewarm water, and keeping nails short. These foundations are important context when considering questions like will benadryl help with eczema, because antihistamines are typically considered add-ons rather than primary eczema therapies.
Understanding Benadryl
Benadryl is widely known as an allergy medication, but people also use it as a sleep aid because it commonly causes drowsiness. That overlap is a big reason it comes up in eczema conversations, especially when itching interferes with rest. To decide whether it is a good choice, it helps to understand what Benadryl is designed to do and what it cannot do.
It is also important to separate two ideas: treating eczema itself versus helping you cope with eczema symptoms. Some medications do not reduce skin inflammation directly but can still be useful for specific situations, such as short-term nighttime relief.
What is Benadryl?
Benadryl is the brand name commonly associated with diphenhydramine, an older antihistamine. Antihistamines are generally used to reduce allergy symptoms like sneezing, runny nose, and itchy, watery eyes. Diphenhydramine is considered a first-generation antihistamine, meaning it can cross into the brain more easily than newer options and therefore tends to cause sedation.
People may reach for Benadryl for eczema when itching feels allergy-like. However, eczema itch is not always driven by the same pathways as seasonal allergies. That difference is one reason results can be mixed from person to person.
How Benadryl Works
Benadryl blocks H1 histamine receptors. Histamine is a chemical involved in many allergic reactions and can contribute to itching and swelling. When histamine is the main driver, blocking its effect can reduce symptoms. Benadryl also has anticholinergic properties, which is one reason it can cause dry mouth, dizziness, and sedation.
In eczema, itching can involve inflammation, skin barrier breakdown, nerve sensitivity, and immune signaling that is not purely histamine-based. So while Benadryl can reduce itch for some people, in other cases it mainly helps by making you sleepy rather than directly calming the skin. This is a key distinction behind the question can benadryl help eczema in a meaningful way.
Types of Benadryl (oral vs. topical)
Benadryl products can be taken by mouth or applied to skin, and the differences matter for eczema-prone skin. Oral diphenhydramine affects the whole body, including the brain, which is why drowsiness is common. Topical diphenhydramine is applied directly to the skin for localized itch, often from bites or mild irritation.
With eczema, topical Benadryl is not always ideal because sensitive, broken, or inflamed skin can react unpredictably. Some people experience irritation or a rash from topical antihistamines, especially when used repeatedly. If you are considering benadryl for eczema, many clinicians are more cautious about topical versions on chronic, inflamed patches than about occasional oral use for nighttime relief.
Does Benadryl Help Eczema?
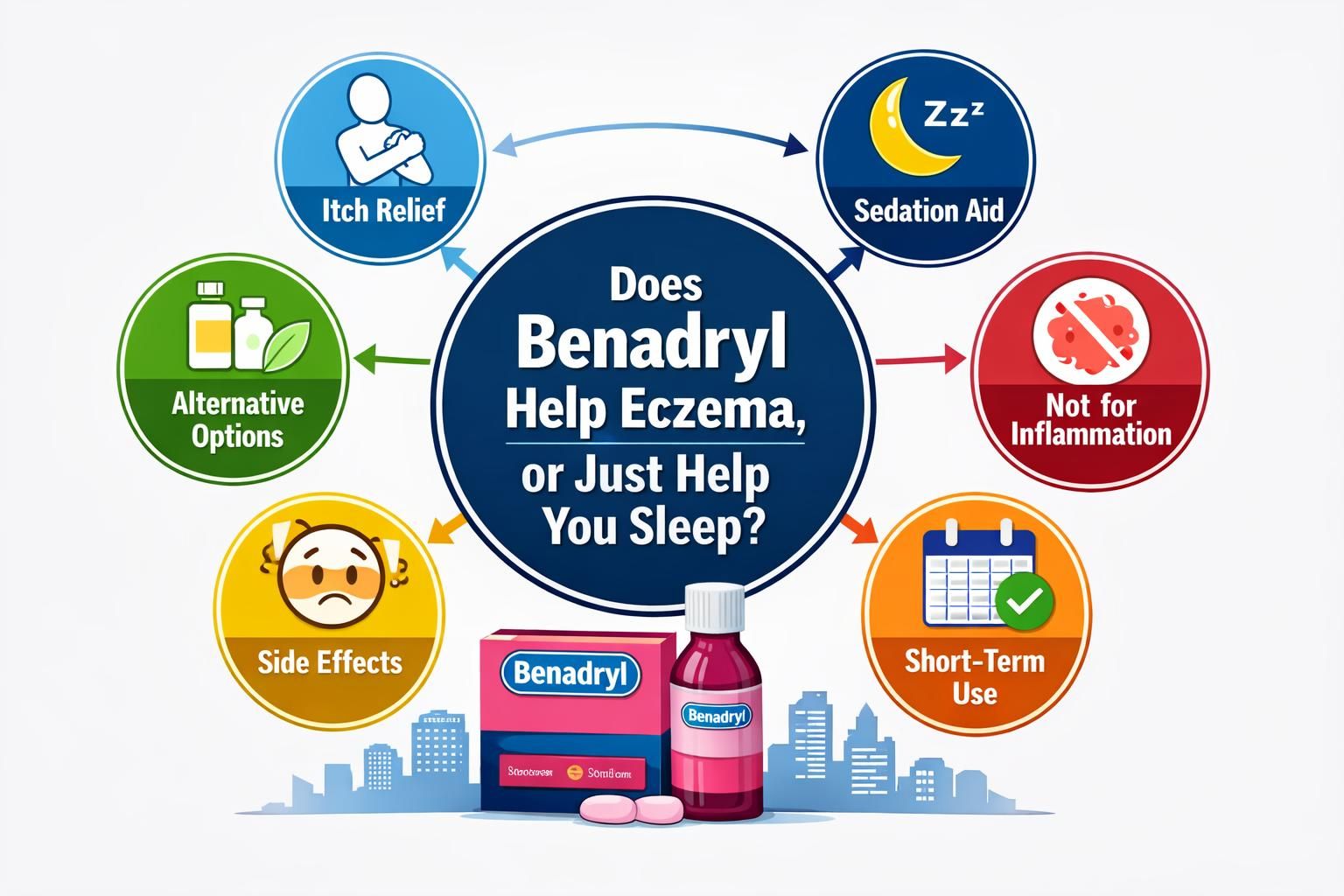
Whether Benadryl helps depends on what you mean by “help.” If the goal is to treat the underlying eczema inflammation, Benadryl is usually not the main tool. If the goal is to get through a rough night by reducing perceived itch or helping you sleep, it may be useful in some situations.
It is also worth considering why the itch is happening at that moment. If you have eczema plus an allergy trigger, histamine may play a bigger role. If your itch is mostly from severe dryness, inflammation, or a flare, the benefit may be limited.
Examining Scientific Evidence
In general, antihistamines are not considered a core treatment for eczema because eczema itch is not consistently histamine-driven. Older, sedating antihistamines like diphenhydramine may help some people sleep through itching, which can reduce nighttime scratching and allow skin a better chance to heal. But sedation is not the same as reducing skin inflammation.
When people ask does benadryl help eczema, the most accurate expectation is that it may provide short-term symptomatic relief for certain individuals, especially at night, rather than reliably improving eczema severity. For daytime itching, the drowsiness can be a drawback, and the anti-itch effect may be modest if histamine is not the main driver.
Efficacy for Eczema Symptoms
Benadryl may help with a few practical eczema-related problems, but it is not a stand-alone solution. Possible benefits include reduced awareness of itching at bedtime, fewer awakenings, and less scratching during sleep. For some people, that can be meaningful, because healing often improves when the skin is not repeatedly traumatized overnight.
On the other hand, Benadryl does not moisturize the skin, repair the barrier, or directly reduce eczema inflammation the way topical anti-inflammatory medications can. If you are asking will benadryl help with eczema during a flare, a more effective strategy is often to pair good nighttime skin care with prescribed or recommended anti-inflammatory treatment, and then consider whether a sedating antihistamine is appropriate for short-term support.
How to Stop Scratching Eczema
Stopping scratching is one of the hardest parts of eczema management because itching is both physical and habit-driven. Scratching can bring brief relief, but it also damages the skin barrier, increases inflammation, and raises the risk of infection. Over time, the skin can thicken and become even itchier, turning a flare into a longer-lasting cycle.
A good plan combines fast itch-calming actions, long-term barrier repair, and behavior changes. The goal is not perfect willpower. It is reducing opportunities to scratch and replacing scratching with safer responses.
The Itch-Scratch Cycle
The itch-scratch cycle starts when inflamed, dry skin sends itch signals. Scratching creates tiny injuries, which worsen barrier damage and inflammation. That damage releases more itch signals, and the cycle repeats. At night, the cycle is often worse because there are fewer distractions, and scratching can happen unconsciously.
Breaking the cycle usually means treating inflammation early, keeping skin well moisturized, and creating physical barriers to reduce damage. It also helps to identify triggers that increase itch, such as heat, sweating, wool-like fabrics, fragranced products, and long hot showers.
Behavioral Techniques to Reduce Scratching
Behavioral strategies work best when they are specific and easy to do in the moment. Instead of telling yourself not to scratch, set up alternatives that reduce damage and calm the nervous system.
- Keep nails short and smooth to reduce skin injury when scratching happens
- Use a cold compress for a few minutes to dull itch signals
- Try pressing or patting itchy areas instead of dragging nails over skin
- Wear soft cotton gloves or sleeves at night if nighttime scratching is a pattern
- Build a quick routine: moisturize, apply prescribed topical medication, then cover with soft clothing
- Use distraction for urge surfing, such as squeezing a stress ball or holding something cold
If you are actively learning how to stop scratching eczema, consistency matters more than intensity. Small changes repeated every day often beat a complicated plan you cannot maintain during a flare.
Role of Antihistamines in Itch Relief
Antihistamines can play a limited, targeted role. Non-sedating antihistamines are often used for allergy symptoms and may help if itching is tied to allergic triggers like hives or allergic rhinitis. Sedating antihistamines, such as diphenhydramine, may help sleep, which indirectly reduces scratching during the night.
This is why people often ask can benadryl help eczema. The most realistic answer is that it can help some people tolerate nighttime itching, but it is not a replacement for eczema treatments that reduce inflammation and repair the barrier. If you find you need antihistamines frequently to cope, that can be a sign your baseline eczema plan needs adjustment.
Potential Side Effects of Benadryl
Side effects matter because eczema can be chronic, and anything used frequently should be evaluated for risks and tradeoffs. Benadryl commonly causes drowsiness, and that can affect driving, work, school, and reaction time the next day. It can also cause dry mouth and constipation, which may be bothersome even with short-term use.
Another consideration is that sedation can mask symptoms without addressing the cause. If itching improves only because you are sleepier, your skin may still be inflamed and worsening underneath. This is one reason Benadryl is usually viewed as an occasional support rather than a primary, long-term strategy for benadryl for eczema.
Common Side Effects
Common side effects of diphenhydramine often relate to sedation and anticholinergic effects. People vary in sensitivity, and some feel groggy the next morning even with a single dose.
Typical issues can include:
- Drowsiness or next-day grogginess
- Dizziness or slowed reaction time
- Dry mouth or dry eyes
- Constipation or urinary hesitation
- Feeling mentally “foggy,” especially with poor sleep or other sedating medications
If you notice side effects that interfere with daily life, it may not be the right tool for managing eczema-related itch.
Risks of Long-Term Use
Long-term, frequent use of sedating antihistamines is generally not a casual decision. Some people develop tolerance to the sleepiness, meaning they may feel less benefit over time. Others may experience ongoing daytime sedation or cognitive dulling. Also, relying on Benadryl nightly can delay more effective eczema management, such as adjusting moisturizers, improving trigger control, or using appropriate anti-inflammatory treatment.
If you feel you need it often, consider discussing your overall plan with a clinician. The goal is to control eczema well enough that you do not need regular sedation to avoid scratching.
Alternative Treatments for Eczema

Eczema treatment works best when it is built around skin barrier repair and inflammation control. Antihistamines, when used, usually sit on top of those foundations. If your main concern is persistent itching, alternatives may address the root causes more directly and provide more consistent relief.
A simple but effective approach often includes gentle cleansing, frequent moisturizing, targeted anti-inflammatory treatment during flares, and environmental changes that reduce irritation. Over time, these steps can reduce flare frequency and intensity.
Moisturizers and Topical Steroids
Moisturizers are a daily essential for eczema because they reduce dryness and help restore the skin barrier. Many people do best with thicker products that seal in water after bathing or handwashing. Consistency is key, especially during colder months or in dry indoor air.
Topical steroids are commonly used during flares to reduce inflammation and itching. Used correctly, they can quickly calm redness and break the itch-scratch cycle. The best option and strength depend on the area of the body and severity. If you are reaching for Benadryl mainly to cope with itch, optimizing moisturizing routines and appropriate anti-inflammatory topicals often provides more direct relief.
Other Oral Medications
When eczema is severe or not responding to topical care, clinicians may consider other oral medications that target inflammation or immune pathways. These are not over-the-counter solutions, and they require individualized medical guidance. In some cases, oral treatments are used for a limited time to regain control of flares, while a long-term maintenance plan is built around topical care and trigger management.
If you suspect allergies contribute to flares, addressing those triggers may also reduce itch. However, eczema is not always allergy-driven, so a careful evaluation helps avoid unnecessary medications and focus on what actually changes your symptoms.
Conclusion
Eczema itching is real, exhausting, and often worse at night. Benadryl can sometimes help by making it easier to sleep and reducing awareness of itch, but it typically does not treat the underlying skin inflammation that drives eczema flares. If you are asking does benadryl help eczema, the most practical approach is to treat Benadryl as a short-term, situation-specific tool rather than a main treatment plan. Start with consistent moisturizing, gentle skin care, and appropriate anti-inflammatory therapy for flares, then add itch-control strategies like cold compresses and nail management. If nighttime itching persists, consider discussing safer, longer-term options with a clinician.
Summary of Findings
Benadryl may reduce nighttime scratching mainly through sedation, not by reliably improving eczema itself. Eczema itch is not always histamine-based, so antihistamines can be hit-or-miss. Topical Benadryl can irritate sensitive skin and is often not ideal for chronic eczema patches. A stronger foundation is barrier repair with moisturizers and targeted anti-inflammatory treatment during flares. Behavioral strategies can also meaningfully reduce damage from scratching.
Final Thoughts on Using Benadryl for Eczema
If you choose to use Benadryl for eczema-related itch, think of it as occasional support, especially when sleep is the biggest problem. Pay attention to next-day drowsiness and avoid using it as a substitute for a complete eczema routine. When you focus on reducing inflammation, restoring the barrier, and breaking the itch-scratch cycle, you are more likely to see lasting improvement than from any single pill.
Disclaimer
This article is for general educational information only and is not medical advice. Eczema can vary widely in cause, severity, and treatment needs. Always follow product labels and talk with a qualified healthcare professional before starting, stopping, or combining medications, especially for children, during pregnancy, or if you have other medical conditions or take other sedating drugs. Seek prompt medical care for signs of skin infection, severe swelling, trouble breathing, or rapidly worsening symptoms.