Eczema can be exhausting: the itching, burning, visible patches, and flare-ups that show up at the worst times. Many people want fast relief and wonder if prednisone helps when topical treatments are not enough. Prednisone can calm inflammation quickly, but it is rarely a simple yes or no. The decision depends on the eczema type, flare severity, and what has or has not worked. This article explains what eczema is, how it is treated, where prednisone fits in, what risks come with it, and what alternatives may help you manage symptoms safely over time.
- Prednisone can reduce severe eczema inflammation quickly, but it is usually a short-term option.
- Most eczema plans start with skin care, trigger avoidance, and topical medications.
- Oral steroids can cause rebound flares when stopped or used repeatedly.
- Non-steroid options include moisturization routines, trigger control, and prescription alternatives.
- Knowing when symptoms are “too much” helps you seek care before complications develop.
Understanding Eczema
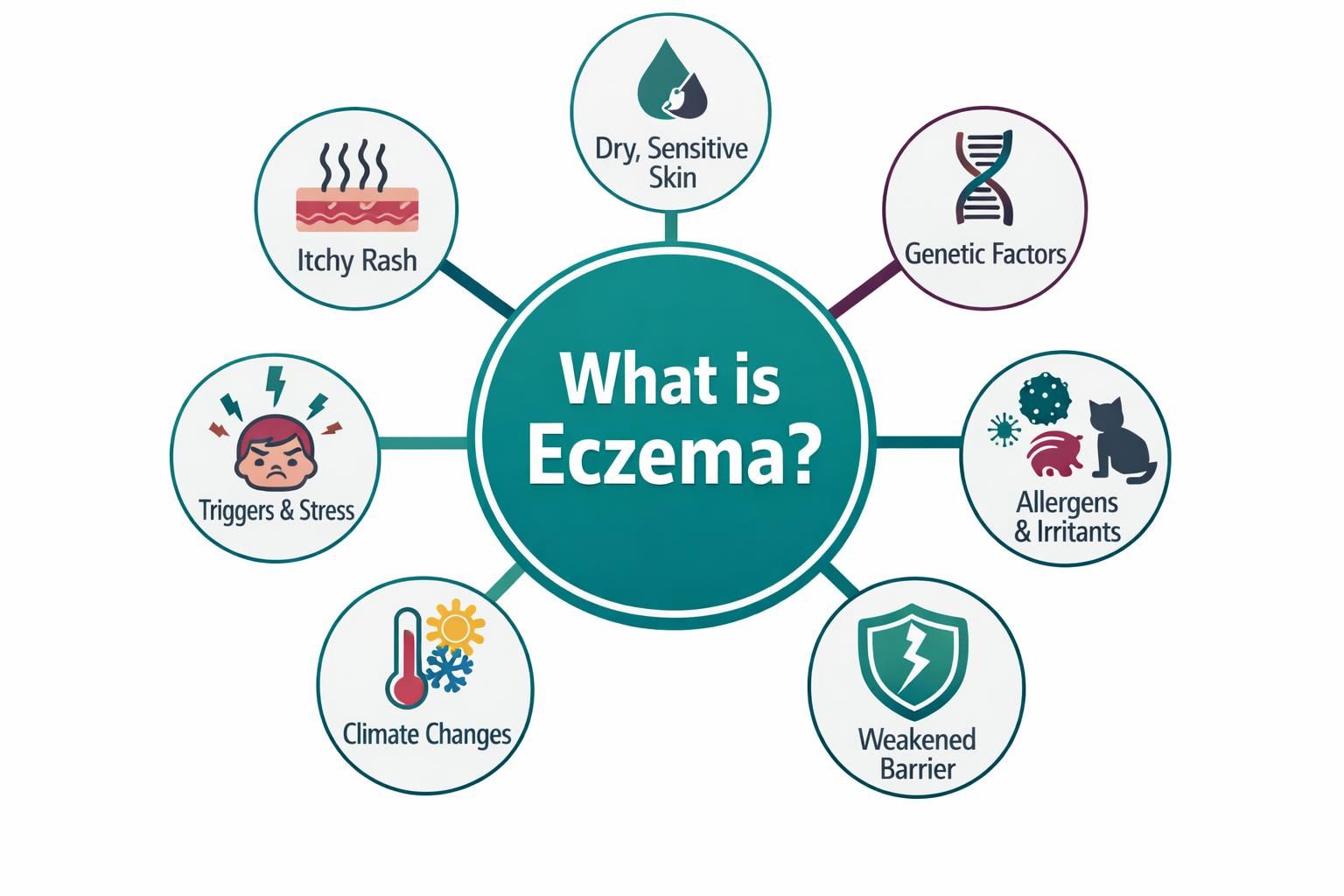
Eczema is an umbrella term for conditions that weaken the skin barrier and make skin reactive. When the barrier is compromised, skin loses moisture and becomes more vulnerable to irritants, allergens, friction, and infection. The result is inflammation that flares, improves, and often returns.
Eczema often starts in childhood but can appear at any age. Severity ranges from mild patches to widespread itching and broken skin that disrupts sleep and daily life. Understanding the basics helps you judge whether systemic treatment like prednisone makes sense.
What is Eczema?
Eczema often refers to atopic dermatitis, but it can also include contact dermatitis, dyshidrotic eczema, nummular eczema, and other patterns. Atopic dermatitis is commonly linked to genetics, immune overactivity, and environmental triggers. Contact dermatitis is driven more by exposures such as soaps, fragrances, metals, or workplace chemicals.
Across types, eczema involves inflammation plus a disrupted outer skin layer. This fuels a loop: itch leads to scratching, scratching damages skin, and damaged skin becomes more inflamed and itchy. Management usually needs both inflammation control and barrier repair.
Common Symptoms
Symptoms vary by age, skin tone, body area, and eczema type. Some flares are dry and scaly; others ooze and crust. Symptoms often improve and return after triggers or stress.
Common symptoms include:
- Itching that may worsen at night
- Dry, rough, or flaky skin
- Red, inflamed patches or darker discolored areas, depending on skin tone
- Thickened skin from long-term rubbing or scratching
- Cracks, bleeding, or painful fissures
- Weeping, crusting, or signs of infection in more severe flares
If you notice warmth, increasing pain, pus, fever, or rapidly spreading redness, it may indicate infection and needs medical attention.
Traditional Treatments for Eczema
Most eczema plans combine daily maintenance with flare control. Maintenance lowers flare frequency and intensity. Flare control calms active inflammation and itching. The best results usually come from gentle skin care, consistent moisturizing, trigger reduction, and medication when needed.
Treatments range from over-the-counter products to prescriptions. Stronger is not always better; consistency matters. Medications may fall short if the skin barrier is neglected or irritants keep returning.
Topical Treatments
Topicals are the foundation because they treat the skin directly. Moisturizers seal in water, reduce micro-cracks, and limit irritant entry. Many people do best moisturizing often, especially after bathing.
Common topical options include topical corticosteroids for flares, topical calcineurin inhibitors, and other non-steroidal prescription creams. Treatment is matched to location and severity, since thin-skinned areas need different choices than thick plaques. Many clinicians also use proactive care: intermittent medication on repeat-problem areas even when skin looks better, alongside daily moisturization to reduce relapses.
Oral Medications
Oral medications are considered when eczema is widespread, severe, or not responding to topical treatment and lifestyle changes. Options may include antihistamines for itch-related sleep disruption, antibiotics when infection is present, or immune-modulating therapies for persistent disease.
Oral corticosteroids like prednisone may be used as short bursts for severe flares causing major discomfort or functional problems. They are generally not preferred long term because of side effects and the risk of return symptoms after stopping. If you need systemic treatment repeatedly, it is a cue to reassess triggers, confirm the diagnosis, and discuss longer-term options with a dermatologist.
Prednisone and Eczema
Prednisone can feel like a reset during a major flare, but it comes with trade-offs. It suppresses inflammation broadly, which can quickly relieve redness, swelling, and itching. The key is when it is appropriate, how long it should be used, and what plan is in place during tapering and after stopping to reduce rebound.
What is Prednisone?
Prednisone is an oral corticosteroid that reduces immune activity and inflammation throughout the body. It is used for many inflammatory and autoimmune conditions because it works quickly.
Unlike topical steroids that act mainly where applied, prednisone circulates systemically. That can help widespread inflammation but increases side effect risk. It is usually prescribed as a short course, sometimes with a taper depending on dose and duration. Tapering may matter because natural steroid production can be suppressed, and stopping suddenly after higher doses can cause problems.
How Does Prednisone Help with Eczema?
Prednisone can rapidly lower immune-driven inflammation that contributes to eczema redness, heat, swelling, and intense itching. As inflammation drops, scratching often decreases, giving damaged skin a chance to heal.
Prednisone does not repair the skin barrier or remove triggers. Without a maintenance plan, symptoms often return after tapering. The goal is to use the relief window to reinforce basics: frequent moisturizing, trigger avoidance, and a clear topical plan to maintain control once prednisone ends.
Will Prednisone Help Eczema in Severe Cases?
In severe cases, prednisone may reduce symptoms enough to restore sleep, decrease widespread redness, and interrupt the itch-scratch cycle. It may be considered when a flare is extensive, inflammation is intense, or other treatments have not provided timely control.
However, severe eczema is also where rebound can be most discouraging. If prednisone is used without a longer-term strategy, symptoms can return quickly and may feel worse if skin is still fragile. Clinicians often reserve prednisone for short-term rescue while optimizing topical treatment, evaluating contact triggers, treating infection, or shifting to other prescriptions better suited for ongoing control.
Risks and Side Effects of Prednisone
Prednisone’s benefits come from broad immune suppression, but that also affects multiple body systems. Side effects depend on dose, duration, and individual health factors. Some appear within days; others develop with repeated or longer use.
Knowing the risks helps you judge whether prednisone is worth it for your flare and recognize when use may be drifting into “too much.” Discuss risks carefully if you have diabetes, high blood pressure, mood disorders, glaucoma, stomach ulcers, or frequent infections.
Short-Term Side Effects
Short courses can still cause side effects, including issues that worsen sleep and stress.
Possible short-term side effects include:
- Increased appetite and fluid retention
- Mood changes such as irritability, anxiety, or restlessness
- Trouble sleeping
- Indigestion or stomach discomfort
- Elevated blood sugar in susceptible individuals
- Temporary rise in blood pressure
- Increased susceptibility to infections while immune response is suppressed
If you feel unusually unwell, develop signs of infection, or experience severe mood changes, contact a clinician promptly.
Long-Term Effects
Long-term or repeated prednisone use raises the risk of serious complications and can create a cycle of brief improvement followed by recurrence, leading to more exposure.
Potential long-term effects include weakened bones, skin thinning and easy bruising, cataracts or glaucoma risk, weight gain, muscle weakness, and suppression of natural steroid production. Immune suppression can increase infection risk. For eczema, another practical risk is delaying a sustainable plan because prednisone works fast. If you need prednisone often, it is a strong signal to revisit diagnosis, triggers, and safer long-term options.
Alternatives to Prednisone

Many people want to avoid systemic steroids or reduce how often they are used. Alternatives include supportive measures that reduce flare frequency and medical therapies that control inflammation with a different risk profile. The right mix depends on eczema type, severity, body areas involved, and your health history.
These strategies work best when consistent: protect the barrier, reduce triggers, calm itching to limit scratching, and treat early so flares do not escalate.
Natural Remedies
Natural approaches can support eczema care, especially for barrier protection and trigger reduction, but “natural” can still irritate. Essential oils and fragranced products commonly worsen eczema-prone skin.
Helpful supportive options include lukewarm bathing with gentle cleansers, frequent use of fragrance-free moisturizers, and humidifying dry indoor air. Wet wraps can help some severe flares by improving hydration and reducing scratching, usually with moisturizers and, when prescribed, topical medication. Patch testing and removing specific irritants can reduce medication needs. Test new products on a small area first.
Can You Cure Eczema Without Steroids?
Many people look for a cure without steroids, but for most chronic eczema types the goal is long-term control, not a permanent cure. Some people have long symptom-free stretches, especially when triggers are identified and barrier care is consistent, but eczema can return with stress, climate changes, illness, or new exposures.
A steroid-minimizing plan often focuses on fragrance avoidance, simplified skin care, daily moisturizing, and quick response to early itch. Medical alternatives may include non-steroidal topicals and other prescription therapies that target inflammation differently than prednisone. Creating a stepped plan with a clinician helps: what to do for mild symptoms, what to do for moderate flares, and what counts as a rescue threshold.
When to Consult a Doctor
Eczema can often be managed at home, but there are times when professional evaluation matters. If you are considering prednisone, medical guidance is important because dosing, tapering, and monitoring depend on your risks. A clinician can also confirm the diagnosis, since fungal infections, psoriasis, scabies, and allergic contact dermatitis can mimic eczema and may worsen with the wrong treatment.
Seeing a doctor also helps you build a long-term plan. Repeated urgent fixes often mean maintenance is not working or the diagnosis needs a closer look.
Signs It's Too Much
“It’s too much” can mean the flare is beyond home care or that the treatment strategy is becoming too risky. Seek medical attention for intense itching that prevents sleep, widespread rash, open cracks that do not heal, rapidly worsening symptoms, or signs of infection.
Prednisone may be becoming too much if you need repeated courses close together, require higher doses for the same relief, or get strong rebound flares after stopping. Other red flags include severe mood changes, major sleep disruption, infection symptoms, or concerning shifts in blood pressure or blood sugar. If your life is being organized around flares, ask about steadier options than intermittent prednisone.
Monitoring Treatment Effectiveness
Monitoring is not only about whether redness fades. It is about function and repeatability: a plan that lets you sleep, work, and live without constant flare anxiety. Tracking a few markers helps you and your clinician adjust before things spiral.
Useful things to monitor include itch severity (especially at night), how often you scratch until skin breaks, how quickly flares return after changes, and which exposures reliably trigger symptoms. Photos can help with week-to-week comparison. Also note non-skin factors like stress, sweating, detergents, and weather changes that may correlate with flares.





