How to Tell If Scar Tissue Is Hiding Skin Cancer
Quick Summary
- Scar tissue from chronic wounds or burns can rarely transform into skin cancer, most often squamous cell carcinoma, so changes in long-standing scars deserve prompt evaluation.
- Warning signs include new growth or a lump, a non-healing ulcer/open sore, color changes (red, brown, black, bluish), persistent itching/bleeding/pain, and hardening or texture shifts.
- Risk increases with chronic sun exposure (scars are more UV-vulnerable), family history of skin cancer, immune suppression, and older age.
- Monitor scars with monthly self-exams and photos, and see a dermatologist for any suspicious change; evaluation may include visual inspection, dermoscopy, and biopsy (punch, excisional, or incisional).
- Treatment commonly involves surgical removal (including Mohs in select areas), with radiation, topical/systemic chemotherapy, or targeted/immunotherapy for certain cases; early detection improves outcomes and follow-up care is important.
Not all scars are created equal—and while most are harmless remnants of past wounds or surgeries, some may hold deeper health concerns. One rare but real concern is that certain scar tissue, especially from chronic wounds or burns, can develop into skin cancer over time. Recognizing when scar tissue warrants a closer look is crucial for early detection and treatment.
This guide will help you understand the differences between normal scarring and potential warning signs of cancerous change, and when it’s time to consult a dermatologist.
Summary
Scar tissue from chronic wounds or burns can rarely transform into skin cancer—particularly squamous cell carcinoma—so changes in long-standing scars deserve prompt attention. Red flags include growth or a new lump, non-healing ulceration, color change, persistent itching/bleeding/pain, and hardening or texture shifts. Regular self-checks, sun protection, and timely dermatology visits (with dermoscopy and biopsy when needed) are key to early detection. Early treatment—often surgical, with radiation, chemotherapy, or targeted/immunotherapy in select cases—significantly improves outcomes.
Understanding Scar Tissue
Scar tissue forms as part of your body’s natural healing process, but not all scars behave the same. Let’s break down what scar tissue really is and how it can vary depending on the injury and healing process.
Scar Formation
When your skin is injured—whether through surgery, burns, or trauma—your body produces collagen to repair the damage. This collagen rebuilds the skin, but often lacks the same structure and strength as normal skin. As a result, scar tissue tends to be thicker, less flexible, and more fibrous. In most cases, scars fade or soften over time, but in some situations, they may remain inflamed or abnormal in appearance, especially if healing was complicated by infection or delayed wound care.
Types of Scars
Scars can vary widely in appearance and behavior. Some types are more likely to raise concerns than others:
- Hypertrophic scars — Raised, red scars that remain within the boundaries of the original wound.
- Keloids — Thick, raised scars that grow beyond the original wound area, sometimes recurring after removal.
- Atrophic scars — Depressed scars, often seen in cases like acne or chickenpox.
- Contracture scars — Usually a result of burns, these can tighten skin and may affect muscles or nerves beneath the surface.
Each type has its own risk profile. For example, long-standing keloids or burn-related contractures can rarely undergo malignant transformation.
Characteristics of Scar Tissue
Typical scar tissue feels different from normal skin. It may be tougher, shinier, or lighter/darker in color. While these traits are usually benign, any sudden changes—such as rapid growth, crusting, or ulceration—could be cause for concern. Scar tissue shouldn’t bleed without cause or develop open sores.
Common Locations of Scar Tissue
Scar tissue can appear anywhere on the body, but areas with repeated friction, sun exposure, or previous injuries are common spots. Watch for scars located on:
- Burn sites (especially unresected or poorly healed)
- Post-surgical sites (chronic non-healing scars)
- Extremities and joints
- Areas that have previously had chronic ulcers or infections
Signs and Symptoms of Skin Cancer
Skin cancer doesn’t always appear as a new mole or freckle—it can also develop within existing scar tissue. Recognizing the signs early is essential for timely treatment and a better prognosis.
Skin Cancer Overview
Skin cancer occurs when skin cells begin to grow abnormally, often triggered by DNA damage from UV exposure or chronic irritation. While the most common types—basal cell carcinoma, squamous cell carcinoma, and melanoma—usually develop on sun-exposed skin, they can also arise in less obvious areas like scar tissue. Recognizing the early signs of skin cancer is crucial for effective treatment. Individuals should familiarize themselves with changes in their skin, including new growths or alterations in existing moles. It’s important to understand how to identify skin tag cancer, as these growths can sometimes be mistaken for benign skin conditions. In addition to regular skin examinations, consultations with a healthcare professional can help determine the appropriate next steps if any concerning changes are observed. Following up on skin cancer blood work results can provide valuable information about the extent of the disease and guide treatment decisions. Early intervention is key, and thorough understanding of both skin changes and test outcomes can lead to better health outcomes.
Different Types of Skin Cancer
Different skin cancers behave in different ways:
- Basal cell carcinoma (BCC): Slow-growing, rarely spreads but can damage surrounding tissue.
- Squamous cell carcinoma (SCC): More likely to arise in chronic scars and wounds; faster growing than BCC and more likely to spread.
- Melanoma: The deadliest form, often appearing as an evolving mole or dark spot but can also arise in scars, especially burn scars.
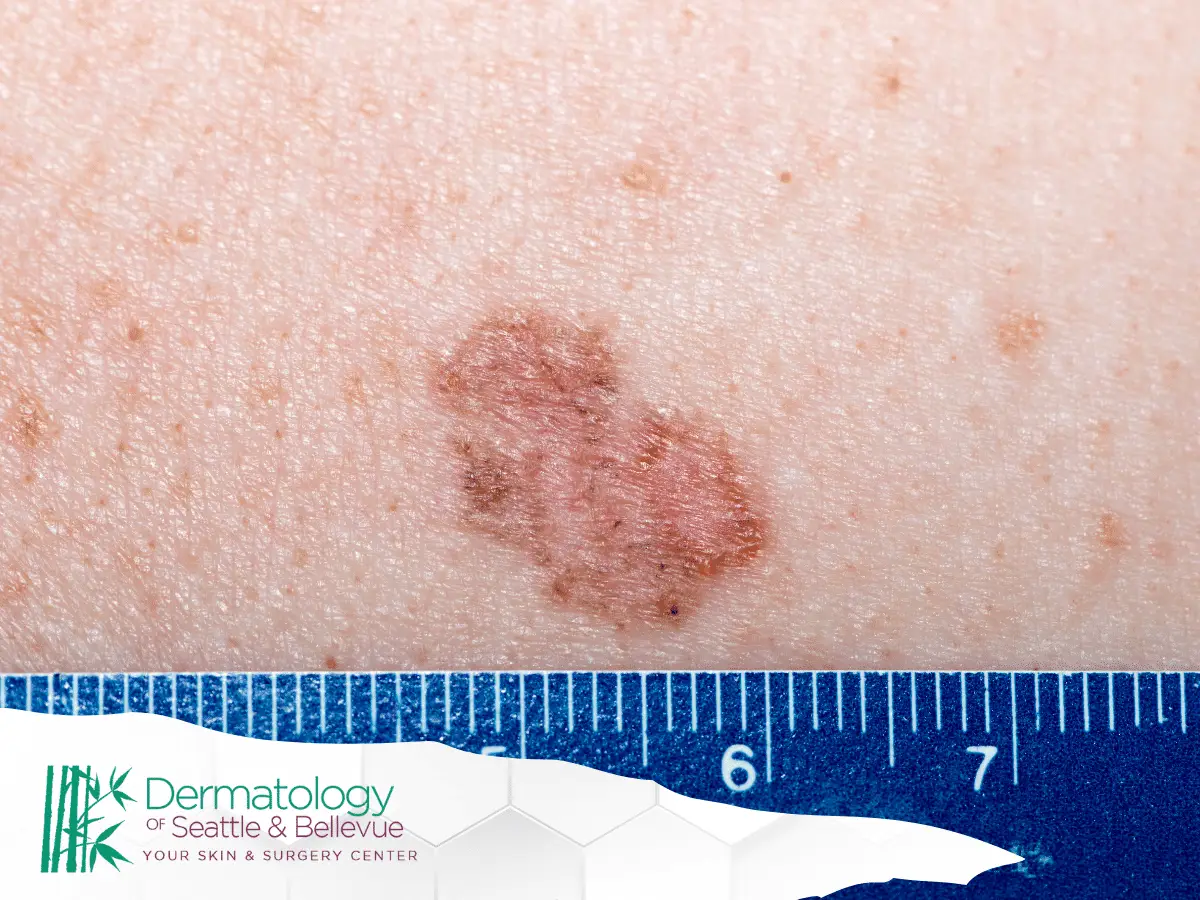
Warning Signs to Look For
When it comes to scar tissue, some warning signs may indicate possible skin cancer:
- A scar that starts to grow, thicken, or develop a lump beneath the surface
- Ulceration or an open sore that doesn’t heal within a few weeks
- Itching, bleeding, or pain in the scar without a known cause
- A change in color, especially if the scar becomes red, dark brown, black, or bluish
- Hardening or rough texture developing over time
These symptoms may seem minor but could point to malignant changes, especially in long-standing scars.
Changes in Existing Moles or Lesions
Even if a mole or lesion seems unrelated to a scar, changes should never be ignored. Look for:
- Irregular borders or asymmetry
- Rapid changes in size or shape
- Unusual colors—especially blue, black, or mixed tones
- Elevation or new bumps forming in flat scars
- Oozing, crusting, or inflammation that persists
Always compare with surrounding skin or past photos when in doubt.
Risk Factors for Skin Cancer
While anyone can develop skin cancer, certain factors increase your risk—especially when it comes to cancer hiding in scar tissue.
Sun Exposure
Chronic sun exposure is a leading cause of skin cancer. UV rays can damage DNA in skin cells—even in old scars. Scar tissue has fewer protective structures than healthy skin, making it more vulnerable to sun-induced mutations. This is especially true for scars in sun-exposed areas like:
- Face
- Neck
- Shoulders
- Arms
Using sunscreen daily, even on healed scars, is an important preventive measure.
Family History
Genetics play a role in your risk. If a close relative has had melanoma, basal cell carcinoma, or squamous cell carcinoma, your odds of developing skin cancer—especially in damaged or scarred skin—may be higher. A family history of skin cancer may warrant more frequent dermatology visits and earlier evaluations of suspicious scar tissue.
Immune System Suppression
Individuals with weakened immune systems—whether from organ transplants, autoimmune diseases, or long-term medication use—face increased cancer risk. Their bodies are less equipped to detect and destroy abnormal cells, including those developing within old scars.
Age
Age is a significant risk factor in the development of skin cancer, particularly in scar tissue. As we age, our skin loses some of its natural ability to repair DNA damage. Combined with years of cumulative sun exposure and slower healing processes, older adults are more likely to experience malignant changes in scarred or previously injured skin.
Evaluating Scar Tissue for Skin Cancer
Not all scars are dangerous—but being vigilant can help you catch early signs of trouble. Evaluating scar tissue regularly is key to identifying cancerous changes before they progress. This section explores how to monitor scars at home and what steps to take if something looks off.
Self-Examination Techniques
It’s important to examine scar tissue just as you would check for new moles or skin spots. Use these self-check techniques:
- Perform monthly skin checks in a well-lit room with a mirror.
- Look for new bumps, ulcers, or sores that don’t heal.
- Note any changes in color, size, or texture of existing scars.
- Take photos of scars to track changes over time.
- Pay attention to discomfort like itching, pain, or bleeding.
When to Seek Professional Evaluation
If a scar begins to change in appearance—whether it darkens, thickens, bleeds, or becomes painful—it’s time to consult a healthcare provider. Don’t wait for multiple symptoms to appear. A sudden change in a long-standing scar or a non-healing wound can signal something more serious. Erring on the side of caution and booking a dermatology appointment ensures timely intervention if cancer is present.
Dermatologist’s Assessment
A dermatologist will visually inspect the scar, assess its texture, color, and behavior, and ask questions about its history. If the scar appears suspicious, further diagnostic tools like dermoscopy may be used to examine skin features that aren’t visible to the naked eye. Dermatologists are trained to distinguish between benign scars and lesions that could indicate malignancy.
Biopsy Procedures
When visual inspection isn’t enough, a biopsy is often the next step. This involves removing a small portion of the scar tissue—or the entire growth—for lab testing. The biopsy determines whether cancerous cells are present and, if so, what type of skin cancer is involved. Types of biopsies used include:
- Punch biopsy (small, circular tissue sample)
- Excisional biopsy (complete removal of the suspicious area)
- Incisional biopsy (partial removal for large lesions)
Visual Inspection
During an exam, dermatologists carefully observe the scar for asymmetry, irregular borders, and unusual pigmentation—hallmarks that may suggest malignancy. They might compare the scar to previous photos or baseline documentation, helping to spot subtle changes over time. Visual inspection remains one of the simplest yet most crucial first steps in identifying suspicious scar tissue.
Texture and Consistency
Scar tissue typically feels firm or rubbery, but if it becomes raised, gritty, or unusually hard or soft, it might indicate something abnormal. Cancerous transformations can create textural irregularities—nodules, ulcerations, or thickened plaques—that deviate from typical scar characteristics. These differences in consistency can help guide decisions about further testing.
Color Changes
Most scars fade with time, but if the tissue darkens, develops mixed shades (brown, red, black, or even bluish tones), or begins to appear mottled, these color shifts could be warning signs. Consistent redness, particularly when paired with inflammation or discomfort, is another cue to seek professional assessment.
Pain and Sensation
While most scars are painless, a sudden onset of pain, tingling, itching, or burning may signal abnormal cell activity beneath the surface. Persistent discomfort in a scar—especially without any recent trauma—can be a red flag. If your scar begins to feel different in any way, it’s important not to dismiss it.
Treatment Options for Skin Cancer
When skin cancer is found in scar tissue, treatment depends on the cancer type, location, and how far it has progressed. Early diagnosis often leads to more favorable outcomes. Treatments aim to remove cancerous tissue, prevent recurrence, and preserve healthy surrounding skin.
Surgical Removal
Surgery remains the most common and effective approach. In most cases, this involves excising the cancerous lesion along with a margin of healthy skin. For high-risk or cosmetically sensitive areas, techniques like Mohs surgery may be recommended to ensure precise removal while sparing healthy tissue.
Radiation Therapy
Radiation therapy may be used when surgery isn’t feasible—especially in cases involving large lesions or difficult-to-reach areas. It involves targeting the affected tissue with high-energy rays to destroy cancer cells. This option is often considered for patients who are not surgical candidates or when cancer recurs after prior treatment.
Chemotherapy
Topical or systemic chemotherapy may be used for certain aggressive or advanced skin cancers. Topical formulations (like 5-fluorouracil) are applied directly to the skin, while systemic chemotherapy is reserved for cancers that have spread beyond the skin. It’s typically part of a more comprehensive treatment plan in such cases.
Targeted Therapy
Targeted therapies are designed to attack specific molecules involved in cancer cell growth. For skin cancer, especially melanoma, treatments like BRAF inhibitors or immunotherapies may be used. These therapies often come into play when standard surgery or radiation isn’t enough or when the cancer has metastasized.
Prevention Strategies
Preventing skin cancer—especially in areas of scar tissue—requires a proactive approach. Because scars can be more vulnerable to cellular changes, protecting your skin and monitoring it regularly are essential for long-term skin health.
Sun Protection
UV radiation is a major contributor to skin cancer, and scars are often more sensitive to sun damage. To reduce risk:
- Apply broad-spectrum sunscreen (SPF 30 or higher) daily, even on cloudy days
- Wear protective clothing (hats, long sleeves) when outdoors
- Avoid peak sunlight hours (10 AM to 4 PM)
- Use zinc oxide or titanium dioxide for scars, which may offer better coverage
Protecting scarred areas from excessive UV exposure helps minimize the chances of skin cancer developing later.
Regular Skin Checks
Consistent monitoring of both normal and scarred skin helps catch abnormalities early. This includes:
- Monthly self-examinations using a mirror
- Looking for new growths, color changes, or itching
- Tracking scar tissue for texture or size changes
- Scheduling annual dermatology checkups
Proper Wound Care
Taking care of wounds from the beginning reduces the risk of abnormal scar development and later complications:
- Keep wounds clean and covered during healing
- Avoid picking or irritating scabs or scar tissue
- Use doctor-recommended ointments or silicone sheets
- Treat any signs of infection promptly
Good wound care can reduce the chances of chronic inflammation or abnormal tissue changes, both of which can raise cancer risk.
Healthy Lifestyle Habits
Overall skin health is closely tied to your general well-being. Support healing and immune response with:
- A diet rich in antioxidants, vitamins A, C, and E
- Hydration and balanced sleep
- Avoidance of smoking, which can impair wound healing
- Limiting alcohol intake
Healthy habits strengthen your body’s ability to repair tissue and may lower the chances of malignant transformation in scars.
Importance of Early Detection
Catching skin cancer early—especially in scarred areas—significantly improves treatment outcomes. Many types of skin cancer, including those that develop in scars, are highly treatable when identified early.
Prognosis of Skin Cancer
When detected early, most forms of skin cancer—including those found in scar tissue—have a favorable prognosis. The type of cancer, depth of invasion, and speed of diagnosis all influence long-term outcomes. For example, early-stage squamous cell carcinoma in a scar can often be fully removed with minor surgery.
Survival Rates
Survival rates for skin cancer vary by type and stage, but early detection typically offers excellent outcomes:
- Basal cell carcinoma: 99% 5-year survival when caught early
- Squamous cell carcinoma: 95% or higher with prompt treatment
- Melanoma: 99% in localized cases, but drops significantly once it spreads
This underscores the importance of monitoring scar tissue for changes and seeking quick evaluations.
Follow-Up Care
After treatment, routine follow-up is critical:
- Schedule regular dermatology visits (every 3–12 months depending on risk)
- Conduct monthly self-checks for new changes
- Use sun protection daily to prevent recurrence
- Maintain clear records of previous diagnoses and treatments
Vigilant follow-up ensures early intervention if another lesion appears, particularly in high-risk individuals or those with a history of abnormal scars.