Mohs
Mohs surgery is a precise surgical technique used to treat skin cancer. During Mohs surgery, thin layers of cancer-containing skin are progressively removed and examined until only cancer-free tissue remains. Mohs surgery is also known as Mohs micrographic surgery.
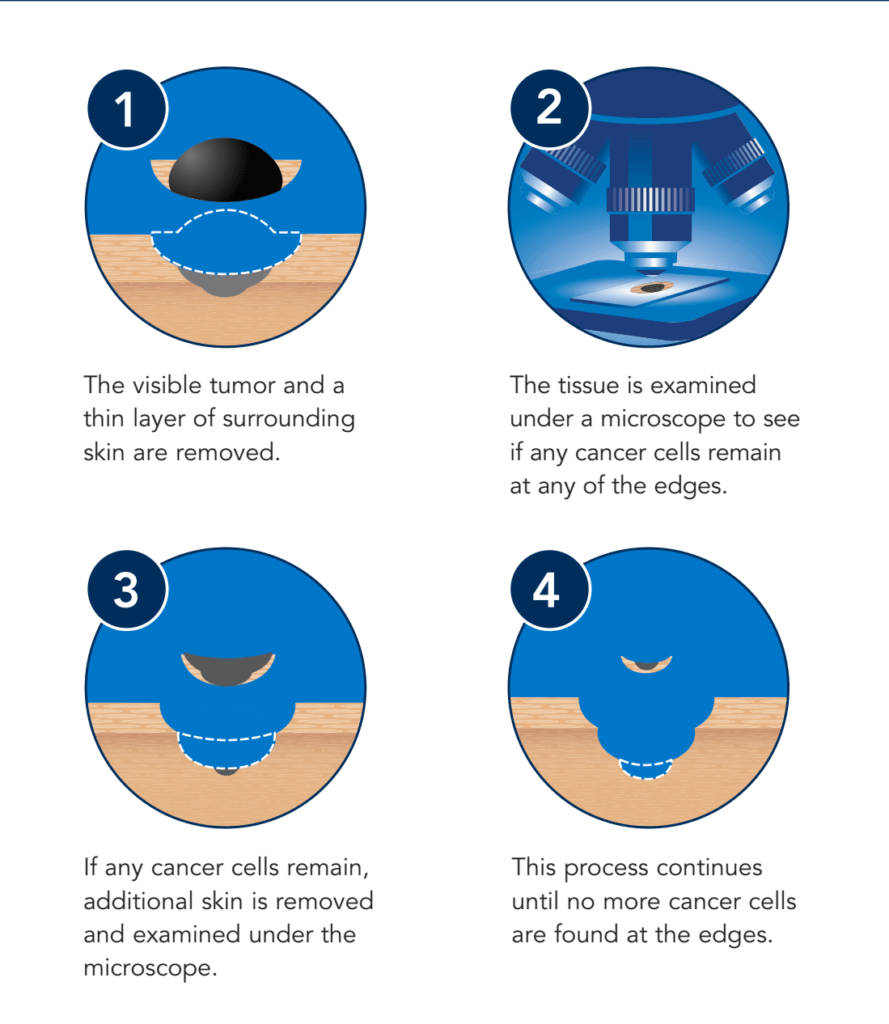
The goal of Mohs surgery is to remove as much of the skin cancer as possible, while doing minimal damage to surrounding healthy tissue. Mohs surgery is usually done on an outpatient basis using a local anesthetic.
Mohs surgery is an improvement to standard surgery (local excision), which involves removing the visible cancer and a small margin of surrounding healthy tissue all at once. Mohs surgery allows surgeons to verify that all cancer cells have been removed at the time of surgery. This increases the chance of a cure and reduces the need for additional treatments or additional surgery.
Additionally we offer Brachytherapy for those who are not a good candidate for Mohs surgery. Learn more about Brachytherapy Here.

